Shivam Goyal
Background
Choroidal naevus is the most common benign intra-ocular tumour. It originates from neural crest derived cells. This lesion is of clinical significance due to risk of visual loss especially if located near the foveola and risk of transformation into malignant melanoma. Traditionally choroidal naevus has been assessed using ultrasound and fluorescein angiography. With advent of new imaging modalities like optical coherence tomography (OCT), fundus autofluorescence (FAF) and OCT angiogram (OCTA) they are being more commonly used to assess naevus.
Low risk naevus is defined as one that is unlikely to transform into melanoma. Features of low-risk naevi are thickness <2mm, presence of drusen, absence of subretinal fluid, absence of orange pigment, absence of symptoms, tumour margins away from optic disc, and echo dense on ultrasound.
It is a common observation that choroidal naevi are rarely seen in younger children. We describe a case of choroidal naevus in a 16-year-old girl referred to our clinic and review of literature to assess its prevalence and outcome in children.
Case Report
A 16-year-old girl was referred to the eye clinic for a fundal lesion in the left eye which was picked up on a routine visit by her optician. The patient was asymptomatic. On examination the visual acuity was 0.0 logmar in each eye. There was no medical or ophthalmic history of note.
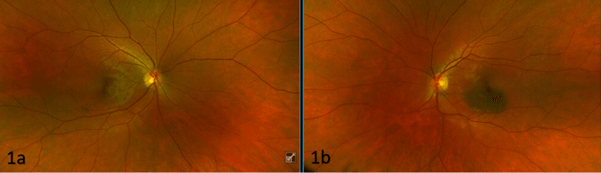
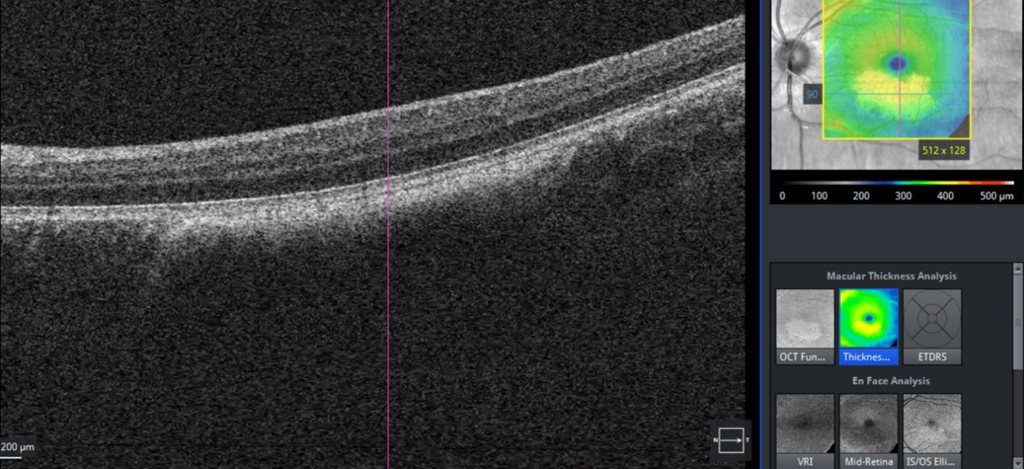
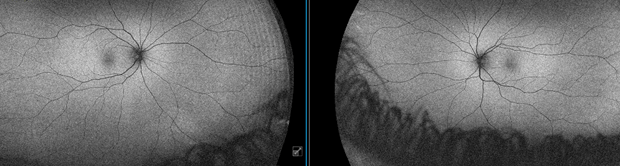
The anterior segment examination was normal. The right eye fundus appearance was normal (figure 1a). The dilated fundus examination of the left eye showed a pigmented lesion with ill defined margins of about 2-disc diameter inferior to the fovea in the macular area (figure 1b). The surface of the lesion had no orange pigment, no drusen and no retinal pigment epithelium alterations (hypoplasia, detachment, atrophy fibrosis). The OCT showed no subretinal fluid over the lesion (figure 2). Autofluorescence of the lesion did not show any bright spots (figure 3). Ultrasound was unable to detect the lesion due to the flat nature. As it had no suspicious features a diagnosis of low-risk choroidal naevus was made and a follow up at one year was arranged.
Discussion
Choroidal naevus is a flat or minimally elevated lesion with (melanotic) or without (amelanotic) pigmentation. It is most often located posterior to the equator (91%) compared to anterior to the equator (9%) (1). The reported prevalence of choroidal naevus varies from 0.2% to 30% in hospital or clinic-based studies whereas in population-based studies the prevalence has ranged from 0.15% to 7.9% because of racial differences in studied population as well as method of detection used (2).
There is not much literature available about the prevalence of clinical features, progression and outcome of choroidal naevus in children. In a recent study published by Ravel et al looking at the prevalence of choroidal naevi in children they found that the incidence increased with age (3). <6 years, 0.47%; 6 years, 0.63%; 12 years, 1.06%; 18 years, 1.79%. That would mean that in the age group of our patient the prevalence according to this study would be around 1.5%.
They also reported that the naevus was unilateral in all cases (48 [100%]), and the majority were melanotic (46 [96%]). Most (36 [75%]) were irregular in shape, with ill-defined margins (45 [94%]). All identified naevi were posterior to the equator. They reported it to be macular in position in 30% of cases. All naevi were small and were not associated with secondary changes (drusen, orange pigment, subretinal fluid).
The majority (18/31 [58%]) of naevi remained stable, with 5 of 31 (16%) demonstrating subtle growth. Malignant transformation was not observed in any of the naevi. Similar to this case series our case did not have any secondary changes and its macular location was similar to commonly reported macular location.
In another large series of 3422 cases describing the clinical spectrum of choroidal naevus related to patient age group at diagnosis (young ≤20 years, mid adult 21-50 years and older adult >50 years), only 2% of choroidal naevi were observed in persons ≤20 years of age (1).
When separately evaluating young, mid-adult, and older adult patients, related symptoms were present in 14%, 12%, and 13%; tumour anteroposterior location was the macula in 34%, 23%, and 20%. The naevus was located posterior to the equator in 91 % of cases. Slight tumour enlargement without melanoma development was found in 3%, 3%, and 4% whereas growth into melanoma was found in 14%, 9%, and 6%.
The important finding of this study was that tumour progression was found even in children who might appear to have an innocent naevus.
Shields et al have reported that one of the most important factors for poor visual acuity in naevi was the sub foveal location (4). They warned that vision loss should be anticipated in patients with sub foveal naevus particularly those with overlying retinal pigment epithelial detachment, foveal oedema and orange pigment over the years. Hence, likelihood of the naevus affecting vision in our case is very low due to its extra-foveal location and no retinal pigment epithelial changes.
According to reported literature choroidal naevi are substantially more prevalent in adults than in children. It is thought that melanocytes originate from neural crest derived melanoblasts that migrate into the uvea. As they migrate they progressively mature and acquire pigment producing capabilities (5), it is hypothesised that choroidal melanocytes undergo a maturation process sometime before adulthood hence their increased prevalence in adults.
Conclusion
It was useful to note that choroidal naevus, though rare, have been reported in children. This information can be given to patient and parents for reassurance. Similar to adults they can be symptomatic and progression to melanoma has been reported. Patients should be warned to contact a specialist if they notice any symptoms. Regular ocular examination of naevi in children should be considered due to risk of transformation to melanoma even if they appear low risk.
References
1. Shields C, Furuta M, Mashayekhi A, Berman E, Zahler J, Hoberman D et al. Clinical Spectrum of Choroidal Naevi Based on Age at Presentation in 3422 Consecutive Eyes. Ophthalmology. 2008;115(3):546-552.e2.
2. Gordon-Shaag A, Barnard S, Millodot M, Gantz L, Chiche G, Vanessa E et al. Prevalence of choroidal naevi using scanning laser ophthalmoscope. Ophthalmic and Physiological Optics. 2013;34(1):94-101.
3. Raval V, Bellerive C, Singh A, Gopinath B, Liew G, Mitchell P. Choroidal naevi in children: prevalence, age of onset, and progression. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2021;25(4):225.e1-225.e6.
4. Shields C. Visual Acuity in 3422 Consecutive Eyes With Choroidal Naevus . Archives of Ophthalmology. 2007;125(11):1501.
5. Schwab C, Zalaudek I, Mayer C, Riedl R, Wackernagel W, Juch H et al. New insights into oculodermal nevogenesis and proposal for a new iris naevus classification. British Journal of Ophthalmology. 2014;99(5):644-649.
