Adeel Mushtaq
Introduction – What is Artificial Intelligence
Artificial Intelligence in the last 5 years, seems to have become a buzzword across all industries in the pursuit of increased efficiency. Its use has transcended cultural and industrial boundaries, an represents a new frontier within technology that can allow for seemingly impossible tasks or problems to now be solved with a fraction of the manpower. There is no generally accepted definition of the concept of AI, however John McCarthy, a computer scientist who coined the term artificial intelligence in the famous Dartmouth Conference in 1956, regarded AI as ‘the science and engineering of making machines that are smart.’ Without taking part in the philosophical argument of what constituted true intelligence, it can be broadly defined as the development and simulation of computer systems that mimic human learning, comprehension, problem solving and, potentially, autonomy.
What is Medical Artificial Intelligence?
Evidence-based clinical decision making by clinicians and other healthcare professionals is based upon past data, whether that be prior mentors, published guidelines or simple personal experience. Simple statistical methods have been able to approach this task by using mathematical equations to derive trends and deviance within data, to then predict the future average. An example of this is linear regression, which attempts to fit a “line of best fit” between two variables on the x and y axis. Artificial Intelligence and Machine Learning uses a similar logic on a much more complex scale. Using training data that have labelled inputs and outputs, the algorithm produces statistical techniques based upon pre-determined biases, to best model the reasoning behind the paired input-output functions. Using this same set of functions, it is then able to take in unlabelled data and produce reasonably accurate outputs that may be previously unknown to the algorithm or to the user. As a result, it is possible that they can uncover associations that humans have not previously recognised. One of the key differences, which poses the greatest asset and threat simultaneously by AI, is that these models can rapidly observe and process inputs and outputs at a scale not previously known. Where a clinician may use their previous experience of treating n number of patients with a condition, AI can compute all records of patients within a defined database, which could be in the thousands. It is then able to learn from all the subtleties of each case, but it can inadvertently, encode in bias that can have the potential to harm a patient or group of patients. A real-world example of this outside of medicine is the scrapped AI algorithm being tested by Amazon as a recruitment selection tool. Using the data submitted by applicants over the previous 10 years, the algorithm concluded that being a woman applicant should inherently be a negative when scoring potential employees.
Artificial Intelligence in Ophthalmology
Within ophthalmology, there is great potential in the application of AI in disease diagnostics/monitoring, as these rely heavily on image recognition and longitudinal image comparison. There have been techniques already developed to detect diabetic retinopathy (1), age-related macular degeneration (2) and glaucoma changes (3) from fundus images, and diseases such as keratitis (4) and cataract (5) from slit-lamp images. Alongside pure diagnosis, models have been trained in the prediction of prognosis and post-treatment predictions of the mentioned diseases.
AI for detection of Diabetic Retinopathy
The rising disease burden of diabetes within both the developing and developed world places unsustainable demands on individuals, carers, heath systems and society. As diabetes causes microvascular non-enzymatic glycosylation, any organ that has a blood supply is susceptible to end-organ damage due to persistent hyperglycaemia. This can range from chronic kidney disease, peripheral neuropathy and resultant non-healing ulcers particularly of the feet, and retinopathy that can lead to blindness if not controlled well. In 2019, it is estimated that 160 million people suffer from some form of DR., and 47 million of these patients had sight-threatening DR (6).By 2045, these numbers are projected to increase to 160.5 million patients, with 44.8 million having vision-threatening DR (7). Early diagnosis of DR can allow for both the clinician and patient time to put in steps to help prevent irreversible vision loss. For this reason, retinopathy screening has been suggested by the WHO, and many developed countries such as the United Kingdom have instated this.
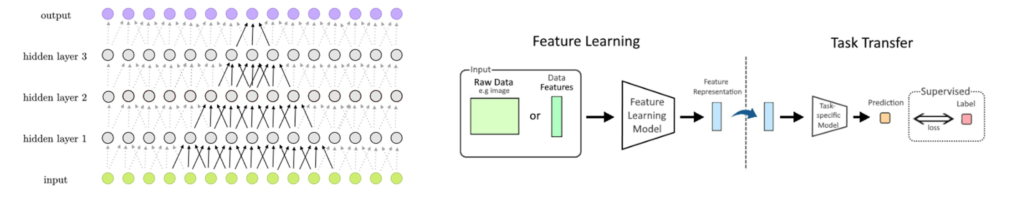
There have been multiple artificial intelligence algorithms developed to achieve accurate detection of DR on fundal imaging. Gulshan et al (8) collected 128,175 fundal images of patients attending for their diabetic retinopathy screening appointment and had them labelled by 54 US-licensed ophthalmologists/ophthalmology trainees. Alongside grading the presence of DR, they also were tasked with grading the image quality and presence and extent of central macular oedema. This data was then used to train a convolutional neural network (CNN) specified for image analysis (See Figure 1). The achieved Area under Curve (AUC) – a marker of algorithm performance based upon prediction of known entities – of 0.99 in internal validation. External validation, meaning testing the algorithm on unknown data, was not performed. Ryu et al developed a CNN using optical coherence tomography – angiography data (OCTA) of 301 eyes and validated its feasibility by training a more traditional machine-learning based classifier (See Figure 1). It managed to achieve an AUC of 0.919 – 0.976, with similar performances seen in external validation (9).
Other convolutional neural networks, such as that reported by Ting et al. (1), Tang et al. (10) and Engelmann et al. (11) shows very promising performance of CNN in the diagnosis and staging of DR, with the later being the most promising as it can report the presence or absence of concurrent retinal diseases, better reflecting the real-world application of this technology.
AI for detection of Glaucoma
Glaucoma is the leading cause of irreversible blindness worldwide, with 4.18 million people aged 50 or over suffering from moderate to severe vision impairment, and a further 3.16 million were blind due to glaucoma (12). Current methods of glaucoma detection involves the assessing clinician to evaluate the neuroretinal margin under slit-lamp or fundal photography, retinal thickness and measured intra-ocular pressure with corneal thickness taken into account. It is notoriously difficult to identify glaucoma in the early stages of the disease, as Primary Open Angle Glaucoma (POAG), Normal Tension Glaucoma (NTG) and Chronic Primary Angle-Closure Glaucoma (CPACG) do not cause eye pain, and the visual field defects caused can be very subtle and not significantly affect the patient’s quality of life enough to seek medical attention. This makes this a perfect area for AI to play a role, as screening using single modality such as fundal photograph, could be possible with a well trained CNN.
Phan et al. (13) reported three deep-learning algorithms that were each able to produce an AUC of 0.9. However, the use of fundal photos that were difficult to label as glaucomatous or not, concurrent retinal diseases and glaucoma-mimics were all excluded thus significantly decreasing the usability of these models themselves. An alternative imaging modality commonly used in specialised glaucoma clinics is three-dimensional spectral domain optical coherence tomography (3D-SDOCT) which utilises the ability of OCT to create a cross section of the retina and reconstructs that information to form a 3D matrix. Ran et al. (14) used this method to train a deep-learning algorithm on and compared its performance with a similar algorithm only trained on 2D line-scanning ophthalmoscopic imaged. They managed to achieve an AUC of 0.969 from three external validation datasets, which was significantly more that the AUC of the 2D-based model (0.831) and individual performance of the glaucoma specialists. As with Phan et al, participants with other ocular or systemic diseases that could affect the retina were excluded, meaning that although this study is very promising and the results impressive, overall generalisability of this algorithm is not available.
As glaucoma is a chronic ocular disease, longitudinal disease progression is important to monitor when making decisions on whether to treat the patient and with what. This poses a difficulty within glaucoma clinics, as it is not common to have the same ophthalmologist see the same patients during follow-up, so accurate documentation is key to basing the current assessment off. Artificial Intelligence here has a great part to play, as it removes the subjectivity of glaucoma assessments and can allow for more data from previous visits to be used in current decision making. Yousefi et al. (15) was able to utilise visual field information from 2085 eyes to train a machine learning algorithm to detect longitudinal change and progression. When tested, it was found to detect progression earlier (3.5 years) than other statistical methods, such as global mean deviation (5.2 years) and point-wise linear regression (3.9 years).
AI in Age-Related Macular Degeneration
Age-related Macular Degeneration (AMD) is a chronic, acquired degeneration of the retina causing significant visual morbidity as it has a bias towards the central vision. Like DR, the disease process is a combination of non-neovascular and neovascular retinal changes that lead to the visual impairment. This is another retinal disease that can be a target for artificial intelligence to help with screening and progression monitoring. Peng et al. (16) utilised the colour fundal photographs collected during the AREDS trial to develop a deep learning model to classify patients already diagnosed with AMD into defined severity category. The resultant DeepSeeNet was successful in detecting large drusen (AUC = 0.94), pigmentary anomalies (AUC = 0.93) and late AMD (AUC = 0.97). The same team developed another algorithm to successfully detect Geographical Atrophy in the same AREDS population, with a reported accuracy of 0.965(17).
There are multiple other algorithms that have been developed, all which have generally shown high success by measured metrics. Dong et al (18) underwent a systematic review and meta-analysis 19 eligible studies using colour fundus photographs to detect age-related macular degeneration. The pooled AUC of the algorithms included in detecting AMD or referable AMD was 0.983. However, a weakness amongst the studies evaluated is that many of them utilised the AREDS population. When selecting the data used in training and testing an AI algorithm, a phenomenon called overfitting needs to be considered. This is when a model is too closely adapted to its training data, causing to perform poorly when approached with new input data.
Conclusion
Artificial Intelligence is paving a new frontier in medicine across specialities. Ophthalmology is uniquely positioned to benefit greatly from the bespoke development and utilisation of AI to allow larger scale screening programmes for retinal diseases. The current state is very promising, with impressive results being produced across the world. However, the key that would allow for AI to penetrate clinical practice is allowing for generalisability of the algorithm i.e. allow it to be able to stage one disease on the background of another.
References
- Ting DS, Cheung CY, Lim G, Tan GS, Quang ND, Gan A, Hamzah H, Garcia-Franco R, San Yeo IY, Lee SY, Wong EY. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. Jama. 2017 Dec 12;318(22):2211-23.
- Dow ER, Keenan TD, Lad EM, Lee AY, Lee CS, Loewenstein A, Eydelman MB, Chew EY, Keane PA, Lim JI. From data to deployment: the collaborative community on ophthalmic imaging roadmap for artificial intelligence in age-related macular degeneration. Ophthalmology. 2022 May 1;129(5):e43-59.
- Li Z, Guo C, Lin D, Nie D, Zhu Y, Chen C, Zhao L, Wang J, Zhang X, Dongye M, Wang D. Deep learning for automated glaucomatous optic neuropathy detection from ultra-widefield fundus images. British journal of ophthalmology. 2021 Nov 1;105(11):1548-54.
- Li Z, Jiang J, Chen K, Chen Q, Zheng Q, Liu X, Weng H, Wu S, Chen W. Preventing corneal blindness caused by keratitis using artificial intelligence. Nature communications. 2021 Jun 18;12(1):3738.
- Keenan TD, Chen Q, Agrón E, Tham YC, Goh JH, Lei X, Ng YP, Liu Y, Xu X, Cheng CY, Bikbov MM. DeepLensNet: deep learning automated diagnosis and quantitative classification of cataract type and severity. Ophthalmology. 2022 May 1;129(5):571-84.
- Burton MJ, Ramke J, Marques AP, Bourne RR, Congdon N, Jones I, Tong BA, Arunga S, Bachani D, Bascaran C, Bastawrous A. The lancet global health commission on global eye health: vision beyond 2020. The Lancet Global Health. 2021 Apr 1;9(4):e489-551.
- Teo ZL, Tham YC, Yu M, Chee ML, Rim TH, Cheung N, Bikbov MM, Wang YX, Tang Y, Lu Y, Wong IY. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021 Nov 1;128(11):1580-91.
- Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, Venugopalan S, Widner K, Madams T, Cuadros J, Kim R. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. jama. 2016 Dec 13;316(22):2402-10.
- Ryu G, Lee K, Park D, Park SH, Sagong M. A deep learning model for identifying diabetic retinopathy using optical coherence tomography angiography. Sci Rep. 2021 Nov 26;11(1):23024. doi: 10.1038/s41598-021-02479-6. Erratum in: Sci Rep. 2022 Dec 5;12(1):21021.
- Tang F, Luenam P, Ran AR, Quadeer AA, Raman R, Sen P, Khan R, Giridhar A, Haridas S, Iglicki M, Zur D. Detection of diabetic retinopathy from ultra-widefield scanning laser ophthalmoscope images: a multicenter deep learning analysis. Ophthalmology Retina. 2021 Nov 1;5(11):1097-106.
- Engelmann J, McTrusty AD, MacCormick IJ, Pead E, Storkey A, Bernabeu MO. Detecting multiple retinal diseases in ultra-widefield fundus imaging and data-driven identification of informative regions with deep learning. Nature Machine Intelligence. 2022 Dec;4(12):1143-54.
- Collaborators GB, Rawal L. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study
- Phan S, Satoh SI, Yoda Y, Kashiwagi K, Oshika T. Evaluation of deep convolutional neural networks for glaucoma detection. Japanese journal of ophthalmology. 2019 May 16;63:276-83.
- Ran AR, Cheung CY, Wang X, Chen H, Luo LY, Chan PP, Wong MO, Chang RT, Mannil SS, Young AL, Yung HW. Detection of glaucomatous optic neuropathy with spectral-domain optical coherence tomography: a retrospective training and validation deep-learning analysis. The Lancet Digital Health. 2019 Aug 1;1(4):e172-82.
- Yousefi S, Kiwaki T, Zheng Y, Sugiura H, Asaoka R, Murata H, Lemij H, Yamanishi K. Detection of Longitudinal Visual Field Progression in Glaucoma Using Machine Learning. Am J Ophthalmol. 2018 Sep;193:71-79
- Peng Y, Dharssi S, Chen Q, Keenan TD, Agrón E, Wong WT, Chew EY, Lu Z. DeepSeeNet: a deep learning model for automated classification of patient-based age-related macular degeneration severity from color fundus photographs. Ophthalmology. 2019 Apr 1;126(4):565-75.
- Keenan TD, Dharssi S, Peng Y, Chen Q, Agrón E, Wong WT, Lu Z, Chew EY. A deep learning approach for automated detection of geographic atrophy from color fundus photographs. Ophthalmology. 2019 Nov 1;126(11):1533-40.
- Dong L, Yang Q, Zhang RH, Wei WB. Artificial intelligence for the detection of age-related macular degeneration in color fundus photographs: A systematic review and meta-analysis. EClinicalMedicine. 2021 May 1;35.
