Ali Adel Ne’ma Abdullah
University Hospital of Wales, UK
Abstract
Uncorrected refractive error (short-sightedness and long-sightedness) is the leading cause of visual impairment worldwide. Traditionally, glasses and contact lenses have been utilised to focus the light onto the retina and hence correct the visual impairment. However, laser refractive eye surgery has emerged as an alternative method to correct refractive error. This article explains the various different types of laser refractive eye surgery by breaking them down into different subtypes of surface and flap-based procedures, followed by evaluating their outcomes, complications, and comparing different procedures against each other.
Introduction
Uncorrected refractive error (short-sightedness and long-sightedness) is the leading cause of visual impairment worldwide (1). It is primarily the result of the axial length of the eye; in short-sightedness (myopia), the eyeball is too long, causing light to be focussed in front of the retina, and in hyperopia (long-sightedness) the eyeball is too short, causing light to be focussed behind the retina (2). Traditionally, glasses and contact lenses have been utilised to focus the light onto the retina and hence correct the visual impairment.
Laser refractive eye surgery has emerged as a more permanent viable alternative to glasses and contact lenses. It involves the use of lasers to reshape the cornea, and hence focus light onto the retina. This article aims to shed light on the different types of refractive laser eye surgery, as well as their visual outcomes and complications.
Flap procedures
A microkeratome (precise corneal blade) or femtosecond laser is used to create a thin flap of corneal tissue. This flap is then lifted out of the way for the remainder of the procedure to continue, before being replaced at the end of the procedure. Broadly speaking, there are three types of flap procedures.
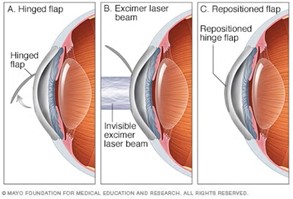
Laser-Assisted in situ Keratomileusis (LASIK) involves the use of a microkeratome or femtosecond laser to create a flap, followed by the use of a laser to remodel the stroma in a finely controlled manner prior to replacing the flap (3) (Figure 1).
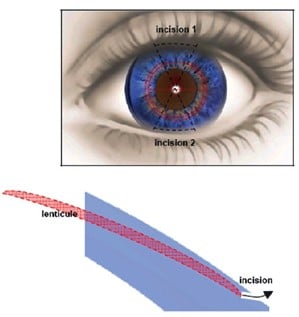
Refractive Lenticule Extraction (ReLEx) is the final flap-based procedure and is subdivided into Femtosecond Lenticule Extraction (FLEX) and Small Incision Lenticule Extraction (SMILE). In FLEX, a flap and a lenticule of corneal stroma are simultaneously cut with a femtosecond laser, followed by manual removal of the lenticule and repositioning of the flap (4). SMILE is a modification to FLEX; a femtosecond laser system is still used to create a lenticule of corneal stroma to be removed, but instead of creating a flap to remove the lenticule, two small incisions are created by the laser system to allow retrieval of the lenticule manually with a spatula and forceps (5) (Figure 2), meaning that technically this procedure is not flap-based.
Surface procedures
These involve the use of an excimer laser to ablate the anterior cornea without creating a flap first. Generally, there are four types.
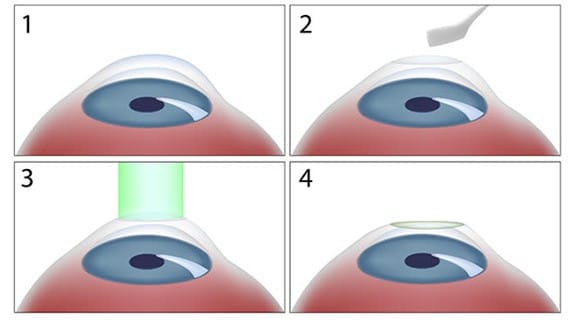
Photorefractive Keratectomy (PRK) first requires removal of the corneal epithelium mechanically using a spatula (6). Once the stroma is exposed, the laser delivers the final result (6) (Figure 3).
Transepithelial photorefractive Keratectomy (TransPRK) is a modification to PRK where the epithelial layer is removed using a laser rather than by scraping manually (7).
Laser-Assisted Sub-Epithelial Keratomileusis (LASEK) is similar to LASIK except that the flap created is much more superficial and contains no stromal tissue, such that the procedure is deemed to be more of a surface ablation procedure rather than flap-based (8). It was developed as an alternative to PRK to address pain caused by PRK’s epithelial debridement (8).
Epipolis laser in-situ keratomileusis (Epi-LASIK) is similar to LASEK except that there is no alcohol used (9).
Outcomes
Studies generally report high levels of patient satisfaction and good visual outcomes after refractive laser eye surgery. Hansen et al. (2015) followed up 81 PRK and LASEK patients for an average of 5 years and found that 96% of patients were satisfied or very satisfied at final follow-up (10). Reported reasons for dissatisfaction included post-operative short- and medium-term haze and myopic regression. Price et al. (2016) performed a 3-year follow-up of 1375 LASIK patients and demonstrated that 88% of former contact lens wearers and 77% of former glasses wearers were strongly satisfied at year 3, compared to 54% in the contact lens control group (11). Reported reasons for dissatisfaction included dry eyes and difficulty driving at night (haloes, starbursts). Schallhorn et al. (2017) demonstrated a 94% satisfaction rate for patients with moderate to high myopia who underwent LASIK and were followed up at 3 months (12). Reported reasons for dissatisfaction included post-operative haloes, glares and starbursts.
As with any surgical procedure, refractive eye surgery carries risks. Some of these are generally considered by patients to be minor nuisances, although they can be very problematic. Dry eye is one of the most common complaints; a recent meta-analysis demonstrated post-operative reductions in tear break up time after LASIK, SMILE, FLEX and PRK, albeit statistical significance was only demonstrated for LASIK and FLEX patients (13). One study analysing LASIK patients demonstrated that 21% complained of dryness; other complaints included glare (20%), haloes (18%) and increased difficulty driving at night (19%) (14).
Severe complications
Some complications, albeit rare, are serious enough to cause significant permanent visual loss. Examples include post-operative infections and corneal ectasia, a devastating protrusion of the cornea as a result of weakened biomechanical strength secondary to surgical thinning (15-17).
Some complications may only envelop after several years. Flaps created in flap-based procedures never fully heal; indeed, it is possible to peel back an anterior corneal flap years later or displace it traumatically (18-19). Furthermore, keratocyte density in the stroma has been shown to decrease after PRK and LASIK (20). Although this has not been shown to have clinical consequences, it is posited that over decades corneal transparency or curvature could be affected (20).
Comparing different techniques
Wen et al.’s (2017) meta-analysis found no statistically significant differences in either visual outcomes (efficacy, safety) or visual quality (higher-order aberrations, contrast sensitivity) among all major forms of laser refractive surgeries (21). Similarly, Tran and Ryce (2018) reported no difference in patient satisfaction or vision-related quality of life among the different techniques (22). However, few high quality and long-term studies exist; more research is required (23). Regarding complications, surface procedures do not lead to aforementioned flap-based complications.
Conclusions
Laser refractive eye surgery is an appealing treatment option for refractive errors owing to its aesthetic allure and reduced dependency on glasses/contact lenses. Visual outcomes are generally good, most patients are satisfied with their procedure, but the short- and long-term risks must be taken fully into account when embarking on this irreversible path.
References
- Verhoeven VJ, Wong KT, Buitendijk GH, Hofman A, Vingerling JR, Klaver CC. Visual consequences of refractive errors in the general population. Ophthalmology. 2015 Jan;122(1):101-9.
- Llorente L, Barbero S, Cano D, Dorronsoro C, Marcos S. Myopic versus hyperopic eyes: axial length, corneal shape and optical aberrations. J Vis. 2004 Apr 22;4(4):288-98.
- Wilkinson JM, Cozine EW, Kahn AR. Refractive Eye Surgery: Helping Patients Make Informed Decisions About LASIK. Am Fam Physician. 2017 May 15;95(10):637-644.
- Sekundo W, Kunert K, Russmann C, Gille A, Bissmann W, Stobrawa G, Sticker M, et al. 2008. First efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: six-month results. J Cataract Refract Surg. 2008 Sep;34(9):1513-20. doi: 10.1016/j.jcrs.2008.05.033. Erratum in: J Cataract Refract Surg. 34(11):1819.
- Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011 Mar;95(3):335-9.
- Lee HK, Lee KS, Kim JK, Kim HC, Seo KR, Kim EK. Epithelial healing and clinical outcomes in excimer laser photorefractive surgery following three epithelial removal techniques: mechanical, alcohol, and excimer laser. Am J Ophthalmol. 2005 Jan;139(1):56-63.
- Fadlallah A, Fahed D, Khalil K, Dunia I, Menassa J, El Rami H, et al. Transepithelial photorefractive keratectomy: clinical results. J Cataract Refract Surg. 2011 Oct;37(10):1852-7.
- Kuryan J, Cheema A, Chuck RS. Laser-assisted subepithelial keratectomy (LASEK) versus laser-assisted in-situ keratomileusis (LASIK) for correcting myopia. Version 2. Cochrane Database Syst Rev. 2017 Feb 15;2(2):CD011080.
- Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol. 2003 Aug;14(4):207-12.
- Hansen RS, Lyhne N, Grauslund J, Grønbech KT, Vestergaard AH. Four-year to seven-year outcomes of advanced surface ablation with excimer laser for high myopia. Graefes Arch Clin Exp Ophthalmol. 2015 Jul;253(7):1027-33.
- Price MO, Price DA, Bucci FA Jr, Durrie DS, Bond WI, Price FW Jr. Three-Year Longitudinal Survey Comparing Visual Satisfaction with LASIK and Contact Lenses. Ophthalmology. 2016 Aug;123(8):1659-1666.
- Schallhorn SC, Teenan D, Venter JA, Schallhorn JM, Hettinger KA, Hannan SJ, et al. Monovision LASIK Versus Presbyopia-Correcting IOLs: Comparison of Clinical and Patient-Reported Outcomes. J Refract Surg. 2017 Nov 1;33(11):749-758.
- Sambhi RS, Sambhi GDS, Mather R, Malvankar-Mehta MS. Dry eye after refractive surgery: a meta-analysis. Can J Ophthalmol. 2020 Apr;55(2):99-106.
- Bailey MD, Zadnik K. Outcomes of LASIK for myopia with FDA-approved lasers. Cornea. 2007 Apr;26(3):246-54.
- Gimbel HV, Penno EE, van Westenbrugge JA, Ferensowicz M, Furlong MT. Incidence and management of intraoperative and early postoperative complications in 1000 consecutive laser in situ keratomileusis cases. Ophthalmology. 1998 Oct;105(10):1839-47
- Wilson SE. LASIK: management of common complications. Laser in situ keratomileusis. Cornea. 1998 Sep;17(5):459-67.
- Wolle MA, Randleman JB, Woodward MA. Complications of Refractive Surgery: Ectasia After Refractive Surgery. Int Ophthalmol Clin. 2016 Spring;56(2):127-39.
- Schmack I, Dawson DG, McCarey BE, Waring GO 3rd, Grossniklaus HE, Edelhauser HF. Cohesive tensile strength of human LASIK wounds with histologic, ultrastructural, and clinical correlations. J Refract Surg. 2005 Sep-Oct;21(5):433-45.
- Dupps WJ Jr, Wilson SE. Biomechanics and wound healing in the cornea. Exp Eye Res. 2006 Oct;83(4):709-20
- Erie JC, Patel SV, McLaren JW, Hodge DO, Bourne WM. Corneal keratocyte deficits after photorefractive keratectomy and laser in situ keratomileusis. Am J Ophthalmol. 2006 May;141(5):799-809.
- Wen D, McAlinden C, Flitcroft I, Tu R, Wang Q, Alió J, et al. Postoperative Efficacy, Predictability, Safety, and Visual Quality of Laser Corneal Refractive Surgery: A Network Meta-analysis. Am J Ophthalmol. 2017 Jun;178:65-78.
- Tran K, Ryce A. Laser Refractive Surgery for Vision Correction: A Review of Clinical Effectiveness and Cost-effectiveness [Internet]. 2018. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; Jun 22.
- Mayo-Wilson E, Ng SM, Chuck RS, Li T. The quality of systematic reviews about interventions for refractive error can be improved: a review of systematic reviews. BMC Ophthalmol. 2017 Sep 5;17(1):164.
