Moussa Al-Rufayie
Introduction
Dacryocystorhinostomy (DCR) is a surgical procedure to treat nasolacrimal duct obstruction, which often results in chronic dacryocystitis and excessive tearing (epiphora). This article provides a comprehensive overview of the procedure, including anatomy and physiology, pathophysiology, historical context, surgical techniques, specific complications, and outcomes (1).
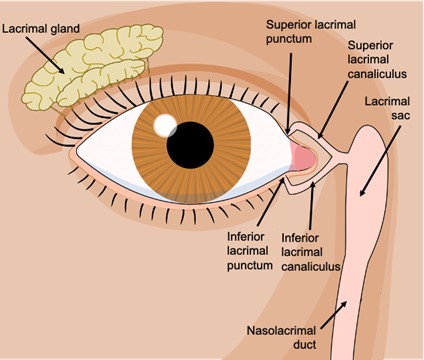
The lacrimal system comprises the lacrimal glands, which produce tears, and the lacrimal drainage apparatus, including the puncta, canaliculi, lacrimal sac, and nasolacrimal duct. Tears produced by the lacrimal glands spread across the eye’s surface and drain through the puncta into the canaliculi, proceeding to the lacrimal sac and finally through the nasolacrimal duct into the nasal cavity (2).
Pathophysiology of Nasolacrimal Duct Obstruction
Nasolacrimal duct obstruction can result from congenital anomalies, infections, inflammation, trauma, or neoplasms. Chronic obstruction leads to tear stagnation, resulting in recurrent infections (dacryocystitis), mucocele formation, and persistent epiphora. The inflammatory response and subsequent fibrosis exacerbate the obstruction, creating a cycle of blockage and inflammation (1).
Presentation and Diagnosis
Patients with nasolacrimal duct obstruction typically present with excessive tearing and recurrent eye infections. Diagnosis involves patient history and clinical examination, including the dye disappearance test and nasolacrimal duct irrigation. The dye disappearance test evaluates tear drainage efficiency by instilling a dye into the conjunctival sac and observing its clearance. Nasolacrimal duct irrigation involves flushing saline through the duct to detect blockages (3). Imaging studies such as dacryocystography and lacrimal scintigraphy confirm the diagnosis and help locate the obstruction. Dacryocystography uses contrast media injected into the lacrimal system, visualised via X-ray to pinpoint obstructions. Lacrimal scintigraphy involves radioactive tracers to assess tear flow dynamics (4).
Surgical Techniques in DCR
The first dacryocystorhinostomy was described by Addeo Toti in 1904, involving the creation of a new passage between the lacrimal sac and the nasal cavity to bypass the obstructed nasolacrimal duct. This procedure has significantly evolved with advancements in surgical techniques and equipment, including endoscopic methods (1).
External DCR
The traditional external DCR involves an incision on the side of the nose to access the lacrimal sac and nasal mucosa. An anastomosis is then created between the lacrimal sac and the nasal cavity. This technique allows direct visualisation of the anatomy and has a high success rate. Surgeons often choose external DCR for its high success rate and excellent anatomical visualisation, making it suitable for complex cases or when a previous endoscopic DCR has failed. However, it can result in visible scarring, infection, haemorrhage (which can be minimised by using vasoconstriction and proper haemostatic techniques), and injury to adjacent structures (5).
Endoscopic DCR
Introduced between the 1980s and 1990s, endoscopic DCR is a less invasive alternative that uses nasal endoscopy to perform the surgery internally, avoiding external scars. It involves creating an opening between the lacrimal sac and the nasal cavity using specialised endoscopic instruments. Surgeons prefer endoscopic DCR for patients who prioritise a minimally invasive approach with no external scars. It is also beneficial in cases where the nasal anatomy or prior surgeries make external access more challenging (6). Complications can include nasal mucosal trauma, granuloma formation, orbital fat herniation, and incomplete drainage (7).
Transcanalicular diode laser assisted DCR
Transcanalicular diode laser-assisted (TCL-DCR) uses a diode laser to create an osteotomy. This precise laser cuts through the bone between the lacrimal sac and the nasal cavity, forming a new drainage pathway. The procedure minimises tissue trauma and bleeding, often resulting in shorter recovery times, as no skin is cut. Surgeons insert a fibreoptic probe through the canaliculus to deliver the laser energy directly to the surgical site. Despite its advantages, it requires specific equipment and expertise, and complications can include burns to surrounding tissue and inadequate osteotomy size (8,9).
Outcomes
External, endoscopic, and laser assisted DCR all show high success rates, generally between 90% and 95%, with arguably no statistically significant difference between the success rates of the different techniques. The choice of technique depends on various factors, including the surgeon’s expertise, patient anatomy, and the specific cause of the obstruction. Endoscopic DCR is often chosen for its minimally invasive nature and lack of visible scars. External DCR is reliable, especially for complex cases, while laser assisted DCR offers precision and reduced trauma, ideal when suitable equipment and expertise are available (10,11).
Conclusion
Dacryocystorhinostomy is a vital procedure for treating nasolacrimal duct obstruction. Advancements in external, endoscopic, and laser-assisted techniques have provided surgeons with multiple effective options, with less complications and high success rates. Ongoing technological improvements are expected to enhance patient outcomes further, making DCR a reliable solution for those suffering from chronic dacryocystitis and epiphora. The availability of different approaches allows for tailored treatments based on individual patient needs and the surgeon’s experience.
References
- Ullrich K, Malhotra R, Patel BC. Dacryocystorhinostomy [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557851/
- Ducker L, Rivera RY. Anatomy, Head and Neck, Eye Lacrimal Duct [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531487/
- Perez Y, Patel BC, Mendez MD. Nasolacrimal Duct Obstruction [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532873/
- Wearne MJ, Pitts J, Frank J, Rose GE. Comparison of dacryocystography and lacrimal scintigraphy in the diagnosis of functional nasolacrimal duct obstruction. British Journal of Ophthalmology. 1999 Sep 1;83(9):1032–5. Available from: https://pubmed.ncbi.nlm.nih.gov/10460770/
- Ali M, Naik M, Honavar S. External dacryocystorhinostomy: Tips and tricks. Oman Journal of Ophthalmology. 2012;5(3):191. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3574519/
- Strong EB. Endoscopic Dacryocystorhinostomy. Craniomaxillofacial Trauma & Reconstruction. 2013 Jun;6(2):67–74. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3721017/
- Ayoob M, Mahida K, Qurat-ul-ain Q, Dawood Z. Outcome and complications of endoscopic dacryocystorhinostomy without stenting. Pakistan Journal of Medical Sciences. 2013 Aug 2;29(5). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858922/
- Awais M, Hassan Naqvi SA, Akram A, Shahid M. Transcanalicular diode laser assisted dacryocystorhinostomy: A breakthrough in the treatment of acquired nasolacrimal duct obstruction. Pakistan Journal of Medical Sciences. 2020 Apr 15;36(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7260931/
- Mor JM, Guo Y, Koch KR, Heindl LM. Transcanalicular Diode Laser-assisted Dacryocystorhinostomy for the Treatment of Primary Acquired Nasolacrimal Duct Obstruction. Journal of visualized experiments. 2017 Oct 13;(128). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5752408/
- Su PY. Comparison of endoscopic and external dacryocystorhinostomy for treatment of primary acquired nasolacrimal duct obstruction. Taiwan Journal of Ophthalmology. 2018;8(1):19. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5890579/
- Panwar S, Lal P, Sukhtankar P. Comparative Analysis of Laser Assisted Endoscopie and Conventional Endoscopie Dacryocystorhinostomy. Medical Journal Armed Forces India. 2006 Jul;62(3):228–30. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4922909/
