Dr Yusuf Abdallah Contact
FY2 Doctor, Wye Valley NHS Trust, UK
Mr Ben While
Wye Valley NHS Trust
Mr Salvi SM
Royal Hallamshire Hospital and Sheffield Children’s Hospital
Abstract
Conjunctival melanoma is a rare ophthalmic cancer which requires a high index of clinical suspicion in order to be managed promptly and appropriately. We present an interesting case of a 74-year-old man with conjunctival melanoma and a red-herring in the form of an ipsilateral peri-ocular benign haemangioma that delayed diagnosis.
Background
Melanoma is defined as a malignant tumour of melanocytes and is usually cutaneous in origin (eyelid melanoma is considered cutaneous). Non cutaneous melanoma is rare, with ocular melanoma accounting for only 3.7% and mucosal melanoma accounting for 1.4% in a study involving 133,209 melanoma cases [1]. Ocular melanoma can be intraocular (uveal melanoma) in 82.5% cases or rarely on ocular surface (conjunctival melanoma). The incidence of conjunctival melanoma is between 0.2 to 0.5 cases per million people and its incidence is rising. [2].
Conjunctival melanomas originate from melanocytes in the basal layer of the epithelium of the conjunctiva. This very rare manifestation of melanoma affects Caucasian patients almost exclusively with equal distribution across both genders and increasing incidence with age over sixty [3,4]. These lesions can arise de novo, from a conjunctival naevus or, more commonly from primary acquired melanosis (PAM). PAM is an acquired pigmentation of the conjunctival epithelium. It refers to flat, brown, lesions of the conjunctival epithelium. The pigment is usually heterogenous and disperse in appearance. It is therefore categorically different to pigmented naevi or other lesions such as those secondary to other causes such as Addison’s disease [5]. PAM most commonly occurs in Caucasian individuals and it is the primary risk factor for conjunctival melanoma as 75% arise from PAM lesions [6,7]. However, most cases of PAM remain benign or occur with only mild atypia [5].
Case presentation
A 74-year-old man presented to his local rural optometrist with a two-year history of increase in size and change in colour of a longstanding pigmented patch on the surface of his right eye, which had been present for over thirty years. He had past ocular history of foreign body removal from welding accidents with consequent corneal scars bilaterally.
He had a benign peri-ocular haemangioma on his right temple and forehead surrounding the orbit which has been present since birth (figure 1).

The optometrist, biased by the patients views, felt that the conjunctival lesion was related to the surrounding haemangioma and made a routine ophthalmology referral, presuming this to be benign in nature.
At his clinic visit, a right eye large, raised, smooth temporal bulbar conjunctival lesion was noted involving the limbus with associated pigment tracking onto the adjacent cornea (figures 2,3). There were no other areas of concern. He had no lymph nodes palpable in his neck region and his past medical history was not significant other than actinic solar keratosis affecting his right hand. A diagnosis of right conjunctival melanoma was made and the patient was referred to the National Sheffield Ocular Oncology Service for definitive management.
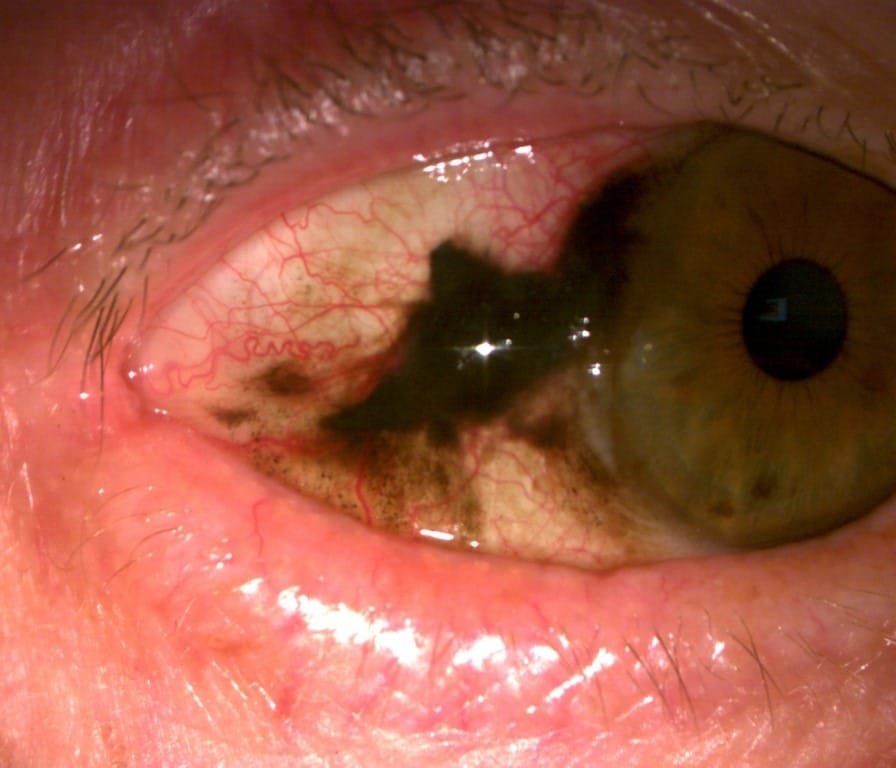
Figure 2 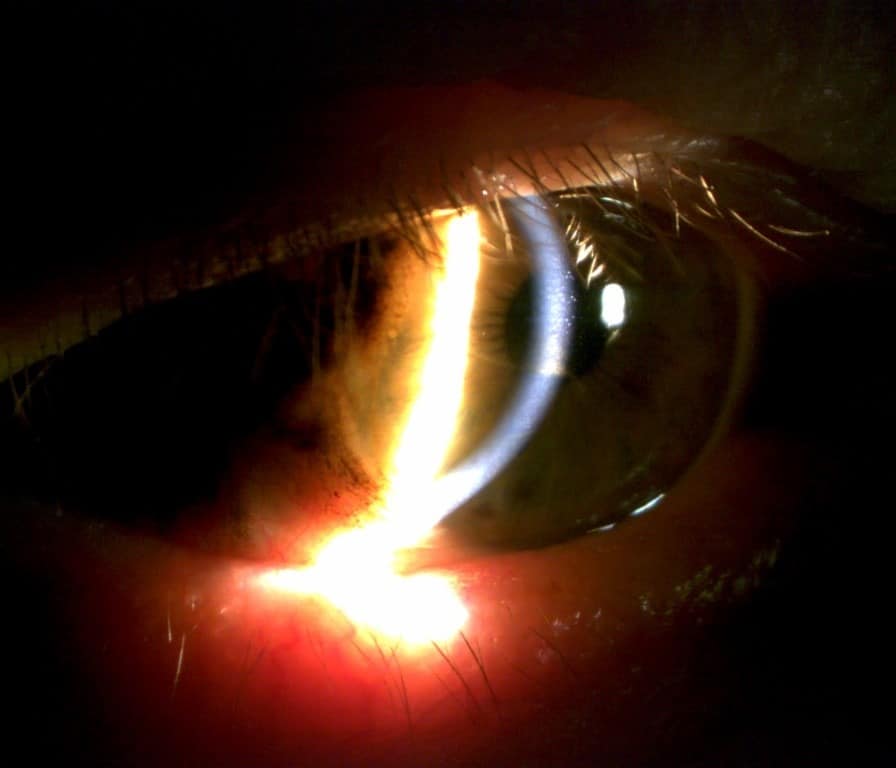
Figure 3
The patient underwent a “non-touch technique” excision of the conjunctival melanoma along with double freeze thaw cryotherapy, alcohol corneal epitheliectomy and amniotic membrane grafting under general anaesthetic. Conjunctival mapping biopsies were also performed. Histopathology confirmed the right bulbar conjunctival melanoma (stage pT1a). The map biopsies demonstrated moderate atypia at 6 o’clock bulbar conjunctiva and mild atypia in the right inferior fornix. The biopsy sites confirmed that the melanoma had arisen from a conjunctival primary acquired melanosis. Eight weeks later, the patient received supplemental ruthenium plaque brachytherapy. Imaging of the head and neck lymph node basin did not reveal any concerning nodes. He remains under long-term follow up and surveillance with the local referring ophthalmology team.
Discussion
Primary acquired melanosis of the conjunctiva (PAM) is a potentially serious melanocytic lesion that can lead to the development of melanoma. PAM and melanoma thus form a spectrum of disease which ranges from benign (PAM without atypia or mild atypia) to premalignant (PAM with moderate or severe atypia) to frankly malignant (invasive melanoma) [5]. PAM with severe atypia is synonymous with melanoma in-situ. The spectrum is based on histological grades of disease and it is clinically not possible to distinguish the various grades of PAM. Hence in patients with suspected PAM, conjunctival map biopsies is required for histopathological analysis to guide management.
The management of PAM remains in flux [2,3,8,9]. Commonly, it is agreed that PAM without atypia and PAM with mild atypia can be managed conservatively. PAM with moderate atypia is treated with adjuvant cryotherapy while PAM with severe atypia is treated with cryotherapy followed by topical chemotherapy such as topical mitomycin C drops. However, the choice of management ultimately depends on the patient and the multi-disciplinary team decision. It is important to note, all patients along the PAM-Melanoma spectrum need to be followed up for life due to the small but everlasting risk of malignant transformation and recurrence.
Untreated, conjunctival melanoma has the potential for metastasis with consequent morbidity and mortality necessitating a high clinical suspicion to enable early diagnosis and treatment. Melanoma must be considered in all patients presenting with complaints of pigmented lesions in the eye especially those on the background of PAM. Most frequently, the bulbar and limbal conjunctiva are affected while the palpebral, forniceal and caruncular conjunctiva are less affected [10, 11].
It is important to evert both the upper and lower eyelids to complete your examination of the conjunctiva. It is also important to bear in mind that pigmentation is not essential to diagnose melanoma as 19% of lesions are amelanotic. Other clinical features which aid in the diagnosis are noted by Wilson et al (2010) including increased vascularity, immobility, and the absence of cysts around the lesions [12]. Possible differential diagnoses are summarised in the differential diagnoses section.
The diagnosis is confirmed with histological examination. It is important to complete conjunctival mapping biopsies to get a full understanding of both the grade and stage of the disease. Cryotherapy is usually combined with surgical excision at first instance as this reduces local recurrence rates [13]. This treatment can be repeated for areas with PAM with atypia as needed.
Medical treatment consists of topical chemotherapeutic agents such mitomycin C and interferon alpha 2b [2,14,15]. Radiation can also be used, most commonly in the form of ruthenium plaque brachytherapy or rarely proton beam therapy, for invasive melanoma either as primary treatment or post surgical excision of melanoma as in our case.
The therapies outlined are not without side effects and these are outlined below [14]. Untreated, there is a risk of intraocular extension and local invasion including CNS extension. Metastatic disease is rare but associated with a high mortality [11, 16].
Differential diagnosis:
- Primary acquired melanosis
- Inhomogeneous pigmentation that is unilateral, more common in females and Caucasians.
- As discussed earlier, PAM with atypia can become conjunctival melanoma.
- Differentiated from melanoma via histological evaluation.
- Nevus
- A variably pigmented, often cystic lump that has been present over a long period of time. It can change with hormonal surges e.g. pregnancy and puberty.
- Complexion-associated melanosis
- Pigmentation that is dusted, predominantly around the limbus and often bilateral. It is seen in darkly pigmented individuals and can increase in size with age.
- Cutaneous melanoma metastasis to the conjunctiva.
- Other nonmelanocytic pigmented lesions:
- Pigmented squamous cell carcinoma
- Foreign body
- Surgical scar
- Silver deposits from eye drops
- Adrenochrome deposition
Treatment side effects:
- Complications:
- Surgical:
- Symblepharon
- Corneal scarring
- Limbal stem cell deficiency
- Infection
- Cryotherapy:
- Damage to neighboring eye structures e.g. cornea, iris, extraocular muscles, eye lids and neighboring conjunctiva.
- This is best avoided with careful cryotherapy applied to the lesion margins while lifting the conjunctiva away from the underlying sclera while applying treatment
- Topical chemotherapy:
- Keratopathy
- Limbal stem cell disease
- Corneal erosions
- Radiotherapy
- Dry eyes
- Loss of lashes
- Focal cataract
- Keratinization of conjunctiva
- Surgical:
Learning points
- Ocular melanoma is a rare condition with sight threatening complications and metastatic potential.
- Ocular melanoma is most common in Caucasian patients over the age of sixty and PAM is the main risk factor.
- It is crucial to evert the upper eyelid and examine the inferior fornix for ‘occult’ lesions
- The mainstay of treatment is via excisional biopsy with various adjuvant therapies.
- Patients require regular lifelong follow up due to the risk of local and systemic recurrence of disease.
References
1. McLaughlin C, Wu X, Jemal A, Martin H, Roche L, Chen V. Incidence of noncutaneous melanomas in the U.S. Cancer. 2005;103(5):1000-1007.
2. Vora G, Demirci H, Marr B, Mruthyunjaya P. Advances in the management of conjunctival melanoma. Survey of Ophthalmology. 2017;62(1):26-42.
3. Wong J, Nanji A, Galor A, Karp C. Management of conjunctival malignant melanoma: a review and update. Expert Review of Ophthalmology. 2014;9(3):185-204.
4. Predrag J, Mihajlovic M, Djordjevic-Jocic J, Vlajkovic S, Cekic S, Stefanovic V. Ocular melanoma: an overview of the current status [Internet]. PubMed Central (PMC). 2013 [cited 18 July 2020]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3693189/
5. Folberg R, McLean I, Zimmerman L. Primary acquired melanosis of the conjunctiva. Human Pathology. 1985;16(2):129-135.
6. Missotten G, Keijser S, De Keizer R, De Wolff-Rouendaal D. Conjunctival Melanoma in The Netherlands: A Nationwide Study. Investigative Opthalmology & Visual Science. 2005;46(1):75.
7. S T, S E, A T, T K. Population-based assessment of clinical characteristics predicting outcome of conjunctival melanoma in whites [Internet]. PubMed. 2002 [cited 18 July 2020]. Available from: https://pubmed.ncbi.nlm.nih.gov/12407149/
8. Herwig M, Wells J. Conjunctival Melanocytic Tumors – EyeWiki [Internet]. Eyewiki.aao.org. 2017 [cited 18 July 2020]. Available from: https://eyewiki.aao.org/Conjunctival_Melanocytic_Tumors
9. Shields C, Shields J. Tumors of the conjunctiva and cornea. Survey of Ophthalmology. 2004;49(1):3-24.
10. Oellers P, Karp C. Management of Pigmented Conjunctival Lesions. The Ocular Surface. 2012;10(4):251-263.
11. Pacheco G, Garcia-Onrubia L, Garcia-Alvarez C, Muñoz M, Garcia-Lagarto E, Perez D et al. A retrospective review of conjunctival melanoma: Presentation, treatment and evolution. Archivos de la Sociedad Española de Oftalmología (English Edition). 2019;94(5):218-224.
12. Shildkrot Y, Wilson M. Conjunctival melanoma: pitfalls and dilemmas in management. Current Opinion in Ophthalmology. 2010;21(5):380-386.
13. Lim L, Madigan M, Conway R. Conjunctival melanoma: a review of conceptual and treatment advances. Clinical Ophthalmology. 2013;:521.
14. Nijhawan N, Hussain A. Conjunctival Melanoma – American Academy of Ophthalmology [Internet]. Aao.org. [cited 18 July 2020]. Available from: https://www.aao.org/oculoplastics-center/conjunctival-melanoma-3
15. Wong J, Nanji A, Galor A, Karp C. Management of conjunctival malignant melanoma: a review and update. Expert Review of Ophthalmology. 2014;9(3):185-204.
16. Shields C. Conjunctival Melanoma Risk Factors for Recurrence, Exenteration, Metastasis, and Death in 150 Consecutive Patients. Archives of Ophthalmology. 2000;118(11):1497.
