Aina Pons1, Nigel Davies1
1Guy´s and St Thomas’ NHS Foundation Trust
Background
Isotretinoin is a retinoid and derivative of vitamin A used to treat severe recalcitrant acne vulgaris. By affecting the cell cycle, cell differentiation, survival, and apoptosis it reduces sebum production, prevents the blockage of pores, and growth of acne-causing bacteria. Additionally, isotretinoin may interact with FoxO1, which may explain a substantial number of isotretinoin’s unexplained actions (1).
Case Presentation
A 26-year-old gentleman was referred to the Eye Department after his optometrist noticed a possible right inferior retinal branch vein occlusion on examination.
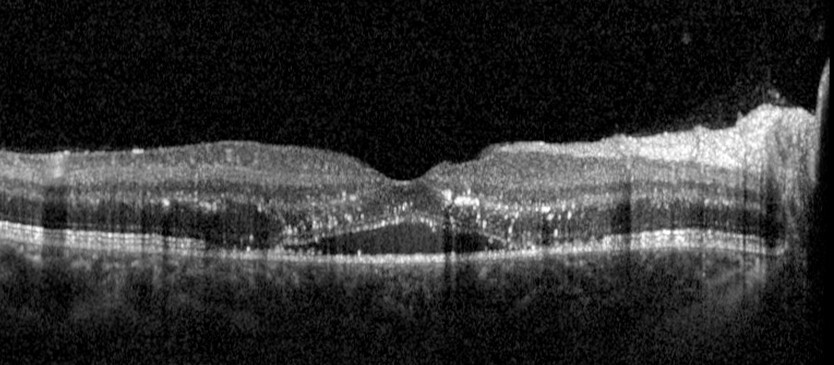
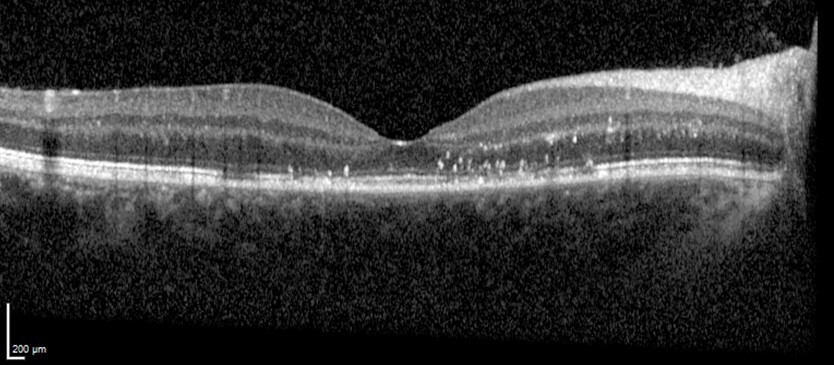
He reported no past medical history nor ophthalmic history and was a life-long non-smoker. He had been receiving treatment for acne with Isotretinoin. In the Emergency Department, he presented with a visual acuity of 0.3 logMAR in the right eye and -0.2 logMAR in the left eye. The intraocular pressure was 13mmHg in both eyes. On examination, the impression was of right inferior venous retinal branch occlusion (Fig 1) (possible evolving CRVO) with cystoid macular oedema (Fig 2A). His blood pressure was 115/85 mmHg and his BM 5.0 mmol/L. He did not present any other physical signs or symptoms on examination. An urgent referral was made to the Haematology Team for further investigations. Anti-VEGF treatment was commenced.

On follow-up, haematological results revealed normal haemoglobin levels and haematocrit as well as normal levels of WBC, platelets, and electrolytes. Thrombophilia tests showed INR=1.1 ratio, APTT=1.2 ratio, and fibrinogen=2.5 g/L. Homocysteine, free protein S and C, and antigen antithrombin were also within normal parameters. Dilute Russell viper venom time (DRVVT) was 1.10 ratio, indicating that lupus anticoagulant (LA) was not present or was not detectable by this method. Anticardiolipin IgG and IgM antibodies were within normal parameters as well as IgG and IgM anti-beta 2 glycoprotein I antibodies.
In a follow-up visit at the Eye Department the visual acuity had improved to 0.0 logMAR in his right eye and -0.3 logMAR in his left eye. The intraocular pressure remained within normal limits in both eyes. Imaging was repeated and showed clear improvement of the cystoid macular oedema after the first anti-VEGF treatment and the course has been continued. (Fig 2B).
Discussion
We report an atypical case of venous retinal branch occlusion in a patient without risk factors for thromboses and with a history of isotretinoin usage. In a previously reported case, a young patient with similar demographic characteristics and presenting a minimal risk for thrombosis developed a CRVO, and the treatment with isotretinoin was thought to have increased the risk of the vaso-occlusive incident after discussion (2).
Thrombocytopenia has been reported in the literature as a rare side effect of isotretinoin use (3). Evidence has been provided that demonstrates that tissue plasminogen activator production is stimulated by isotretinoin, and that this, together with falling tissue plasminogen activator inhibitor levels, may accelerate fibrinolysis (4,5).
Additionally, some authors have reported cases of increased bleeding risk when using isotretinoin in patients with haemophilia A with exacerbation of the patient’s bleeding tendency (6). However, previous literature has reported that isotretinoin can induce hyperhomocysteinaemia and decreased serum folic acid levels, which may be a risk for cardiovascular disease and thrombosis (7). Thrombosis also appears as a potential rare side effect of isotretinoin use (3). We hypothesise that this was the cause of the venous retinal branch occlusion in our patient.
In the same previous case, DNA testing was used to reveal that the patient was a heterozygous carrier of the G20210A mutation of the prothrombin gene. However, no genetic testing was undertaken for our patient which somehow limits the interpretation of risk when under treatment with isotretinoin.
In our case, haematology results and thrombophilia revealed no added risk for thrombosis, but an underlying genetic mutation could predispose certain patients to develop coagulation disturbances when taking isotretinoin (1). The association with isotretinoin should be taken into consideration by medical practitioners but interpreted with caution. Further research should investigate this association and causality should be explored.
References
1) Go.drugbank.com. 2022. Isotretinoin: Uses, Interactions, Mechanism of Action | DrugBank Online. [online] Available at: <https://go.drugbank.com/drugs/DB00982> [Accessed 6 September 2022].
2) Labiris, Georgios, et al. Association between isotretinoin use and central retinal vein occlusion in an adolescent with minor predisposition for thrombotic incidents: a case report. Journal of Medical Case Reports, 2009, 3.1: 1-5.
3) Webmd.com. 2022. Common and Rare Side Effects for Isotretinoin. [online] Available at: <https://www.webmd.com/drugs/2/drug-6662/isotretinoin-oral/details/list-sideeffects> [Accessed 6 September 2022].
4) Dootson, G. M.; Keidan, J.; Harper, P. L. The influence of isotretinoin upon fibrinolysis in patients with acne. British Journal of Dermatology, 1995, 133.1: 66-70.
5) Kaptanoglu, Asli Feride, et al. Effect of isotretinoin on prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT). Journal of dermatological treatment, 2013, 24.4: 272-274.
6) Dotson, G. M.; Keidan, J.; Anderson, J. A. R. Exacerbation of bleeding tendency in a patient with haemophilia A, during treatment with isotretinoin. British Journal of Dermatology, 1992, 127.2: 186-187.
7) Van, Thanh Le Thai, et al. Efficacy of oral low-dose isotretinoin in the treatment of acne vulgaris in Vietnam. Open Access Macedonian Journal of Medical Sciences, 2019, 7.2: 279.
