Abdullah A Cheema1, Connor Qiu2, Babar Khan3
1Royal Glamorgan Hospital
Llantrisant
Wales2Royal Free London NHS Foundation Trust
Pond Street
London3Babar Khan
Department of Ophthalmology
North Road Eye Clinic
Bronglais Hospital
Aberystwyth
Senile or degenerative retinoschisis is an uncommon condition usually seen in persons over the age of forty years (1,2). Retinal breaks involving the outer or inner layers of a retinoschisis cavity may occur during the natural history of the condition (3). We describe a patient, who developed retinal breaks at the inner and outer layers of the schisis cavity following trauma, resulting in an unusual appearance of dialysis at edges of retinoschisis, requiring laser photocoagulation to prevent retinal detachment. No previous report describing such features has been reported in the literature.
Case report:
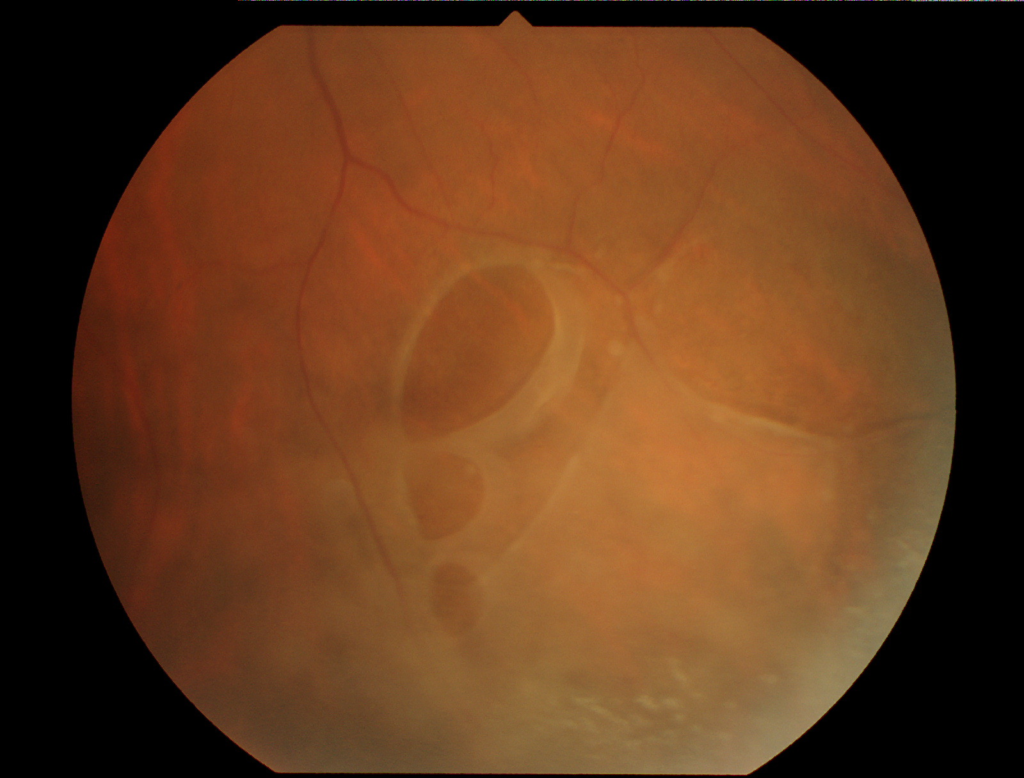
A seventy years old healthy male presented to our hospital, complaining of blurred vision in his left eye with a 3 day history of blunt trauma (hit with shoe) in his left eye. Ocular assessment of the right eye was normal, except for an area of retinal elevation in the infero-temporal quadrant, characteristic of degenerative retinoschisis with presence of yellowish-white flecks on the surface of the retinoschisis cavity. The affected left eye showed visual acuity of 6/60 improving to 6/24 with pinhole. Pupil reactions and intraocular pressure were normal. There were signs of mild anterior uveitis and pigment cells were seen in the anterior vitreous. Fundal examination revealed a peripapillary haemorrhage (Figure 1) nasal to the disc, while an area of retinoschisis similar to the right eye was seen in the infero-temporal quadrant of the retina.

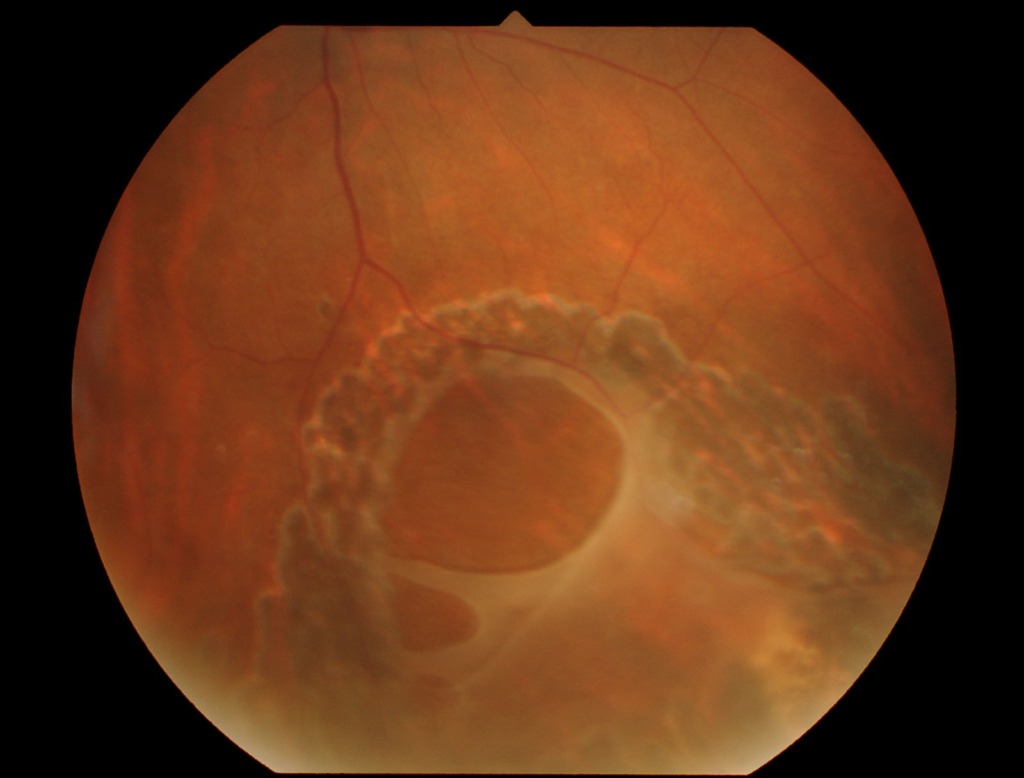
However, retinal breaks in the inner and outer layers of the schisis cavity, giving an appearance of dialysis along the superior margin of the retinoschisis were noted (Figure 2) The full thickness retinal holes in retinoschisis exposed a large area of retinal pigment epithelium establishing a communication between the sub-retinal space, schisis cavity and vitreous. No evidence of posterior vitreous detachment was noted.
The patient was started on topical steroid drops and closely monitored over the following weeks. During the first week, anterior uveitis improved and fluid from the schisis cavity gradually resolved, resulting in almost complete flattening of the cavity. A procedure of argon laser photocoagulation to circumvallate the retinal breaks was undertaken as prophylaxis against retinal detachment. At the last follow-up (3 months) the retina remains stable with visual acuity of 6/6. The schisis cavity has completely resolved, with good laser scars around the retinal breaks. (Figure 3)
Discussion
A blunt injury usually results in anteroposterior indentation and equatorial expansion of the globe, producing shearing forces and traction along the borders of the vitreous base, causing retinal dialysis (4,5). Retinal breaks can also occur at sites of focal scleral impact or from posterior vitreous avulsion (6).
Our patient had peripapillary choroidal haemorrhage, and unusual appearance of retinal holes giving an appearance of dialysis along the superior margin of the retinoschisis cavity. This scenario following blunt trauma, probably arose as a result of shearing and traction at the thin margins of the retinoschisis cavity. However, such forces were not strong enough to cause retinal dialysis or tears in the nonpigmented epithelium of the pars plana. The fluid in the schisis cavity absorbed as large outer layer breaks provided communication between the schisis cavity and the subretinal space. We performed circumvallation of retinal tears following the absorption of schisis cavity fluid to prevent the possibility of retinal detachment, which could develop following progressive liquefaction of vitreous that could allow fluid to enter the subretinal space through the retinal tears.
References:
- Byer NE. Clinical study of senile retinoschisis.Arch Ophthalmol. 1968 ;79:36-44.
- Rutnin U, Schepens CL. Fundus appearance in normal eyes. 3. Peripheral degenerations.Am J Ophthalmol. 1967 ;64:1040-62.
- Byer NE. Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology. 1986;93:1127-37.
- Weidenthal DT, Schepens CL. Peripheral fundus changes associated with ocular contusion. Am J Ophthalmol. 1966 ;62:465-77.
- Delori F, Pomerantzeff O, Cox MS. Deformation of the globe under high-speed impact: it relation to contusion injuries. Invest Ophthalmol. 1969 ;8:290-301.
- Cooling RJ. Traumatic retinal detachment–mechanisms and management. Trans Ophthalmol Soc U K. 1986;105 :575-9.
