Shi Pei Loo1, Kanna Ramaesh2
1Foundation Year Doctor, NHS Greater Glasgow and Clyde
2Consultant Ophthalmologist, Tennent Institute of Ophthalmology, NHS Greater Glasgow and Clyde
Introduction
Endophthalmitis is a rare but devastating, sight-threatening complication of intraocular surgery and intravitreal injections (IVIs). The visual outcome of postoperative endophthalmitis is poor. High volumes of cataract surgery are performed worldwide, and the incidence of postoperative endophthalmitis is relatively low. This relatively very low incidence of endophthalmitis can be attributed to two factors. It is a well-established fact that pre-operative cleaning of the conjunctival sac and the eyelids with povidone-iodine (PI) for up to three minutes has contributed to the reduction of endophthalmitis (1-3). The second factor contributing to the decrease in endophthalmitis is the administration of intra-cameral antibiotics at the end of surgery.
PI consists of the polymer povidone complexed with triiodide (I3-), and it slowly releases free iodine, which has a broad range of antimicrobial, antifungal, antiprotozoal and antiviral actions (4). Current European Society of Cataract and Refractive Surgeons (ESCRS) guidelines recommend the application of 5-10% PI to the cornea, conjunctival sac and periocular skin for a minimum of three minutes before cataract surgery (5).
PI was introduced in the 1950s. Before this, Argyrol (a mild silver protein) was commonly used to clean the eye (6). The post-operative endophthalmitis rate was high during the pre-PI era (7). However, a challenge to administering PI before ophthalmic procedures arises when patients voice concerns regarding an “iodine allergy”. This usually occurs when patients with previous adverse reactions to iodine-containing compounds, commonly shellfish and iodinated contrast media, report being allergic to iodine (8). In a 2020 survey of consultant ophthalmologists, 323 respondents (97.3%) reported encountering a patient with a self-reported iodine allergy, highlighting that this is a commonly encountered scenario in ophthalmology. In the same survey, 74.1%, 38% and only 11% of respondents would continue with PI prophylaxis in patients with reported seafood, iodinated contrast media and iodine allergies, respectively (9), suggesting that PI is withheld in many cases due to concerns regarding iodine cross-reactivity between PI and iodine-containing compounds. In this commentary, we aim to discuss how “iodine allergy” is a misconception. Iodine is essential for many physiological processes and is not the component responsible for adverse reactions to seafood or iodinated contrast media. A true allergy to PI is rare; in most cases, patients are experiencing irritant reactions. PI mustn’t be withheld in cases of reported “iodine allergy” as this increases the risk of endophthalmitis and risks ocular morbidity.
Clinical Definition of Allergy
Allergy occurs when a person reacts to substances in the environment that are harmless to most people. This is a reaction mediated by the immune system. These substances are known as allergens and are found in dust mites, pets, pollen, insects, ticks, moulds, foods and some medications (10). Atopy is the genetic tendency to develop allergic diseases. When atopic people are exposed to allergens, they can create an immune reaction that leads to allergy. The manifestations of allergy can vary from mild itch to severe anaphylaxis. The clinical manifestations include allergic rhinitis (hay fever), conjunctivitis, eczema, urticaria, bronchospasm, laryngeal oedema and anaphylaxis (11). The genesis of allergy starts with the allergen (such as pollen) entering the body, which triggers an IgE antibody response. The antibodies attach themselves to mast cells. When the allergen comes into contact with the antibodies, the mast cells release histamine and other kinins. These chemical mediators trigger tissue and inflammatory responses that manifest clinically with allergy symptoms (12). Similar reactions can occur to some chemicals and food additives. However, if they do not involve the immune system, they are known as adverse reactions, not allergies (11).
“Iodine Allergy”
Patients are usually told that they have an “iodine allergy” when they experience adverse reactions to iodine-rich compounds such as seafood and iodinated contrast dye (8). However, “iodine allergy” is a misconception as an allergy to iodine would be incompatible with life. Iodine is an essential trace element synthesising the thyroid hormones triiodothyronine (T3) and thyroxine (T4). These hormones play a crucial role in stimulating the development of the skeletal and central nervous systems in utero and infants, and in regulating protein synthesis, growth and metabolism throughout life (13). Iodine can be found in various foods such as seaweed, seafood and eggs and in iodinated salts and dietary supplements. The recommended daily iodine intake for adults is 140 mg (14). Iodine deficiency, which is endemic in regions such as the Himalayas and South Asia, can cause hypothyroidism, leading to the development of a goitre and systemic symptoms such as fatigue, cognitive changes, constipation and, in severe cases, death (15). Cognitive development is adversely affected by severe iodine deficiency during childhood (16). In summary, an “iodine allergy” is not possible as iodine is necessary for many physiological processes in the human body, and its deficiency would lead to adverse health effects that can be fatal.
Seafood Allergy
The literature suggests that PI is not used as postoperative endophthalmitis prophylaxis in most cases of reported seafood allergies (9). This could be due to concerns regarding seafood’s high ionic content and the potential iodine cross-reactivity with PI. However, these allergic reactions are not due to iodine but to protein allergens in the seafood. Iodine is a simple molecule that does not contain the antigenicity to trigger an immune response (17). In shellfish, tropomyosin is the primary protein allergen for all consumable crustaceans and molluscs. Other shellfish protein allergens identified include arginine kinase, myosin light chain, and sarcoplasmic binding protein (18). Allergic reactions to fish are likely triggered by the protein parvalbumin (17). These allergens cause IgE sensitisation but are not present in PI (18). Hence, PI should not be withheld in cases of seafood allergy as there is no cross-reactivity between seafood and PI.
Iodinated Radiocontrast Dye Allergy
Adverse reactions to iodinated radiocontrast dyes can be classified into acute reactions, which occur within one hour of exposure, and delayed reactions, which occur an hour to one week after. Severe acute reactions can mimic anaphylactic reactions with features including urticaria, bronchospasm and cardiovascular collapse (19). These extreme reactions, however, are termed anaphylactoid reactions as they occur due to the degranulation of mast cells and basophils after direct stimulation. No immune memory is formed in these reactions as they are not IgE-mediated; hence, there is no risk of cross-reactivity with PI. Moreover, these anaphylactoid reactions are not triggered by the dye’s iodine but by the contrast dye’s hyperosmolarity relative to blood. Most clinical settings now use non-ionic, low-osmolality contrast media instead of ionic, high-osmolality ones, as the low-osmolality contrast media have a minor irritant effect and are associated with a fivefold decrease in severe acute reactions (20)—delayed reactions to iodinated radiocontrast dye commonly present with mild symptoms such as rash and pruritis. A literature review found that most case reports did not show iodine cross-sensitivity between radiocontrast media and other iodine-containing compounds. These case reports mainly described positive skin, patch and intradermal tests for the dyes but negative tests for potassium iodide and iodine (19). Hence, adverse reactions to iodinated contrast dyes should not be a contraindication to PI administration, as other allergens in the dye are causing these reactions and not iodine itself.
Reactions to Povidone Iodine
Reactions to PI include irritant reactions, contact dermatitis and rarely anaphylaxis. These reactions are due to povidone and not iodine; hence, a reported allergy to iodine or iodine-containing compounds alone should not be a contraindication to administering PI (17). Irritant reactions are frequently misdiagnosed as allergic contact dermatitis as both can present similarly with a rash, and patch test results may be false positives due to irritation from PI. A study using 1% PI on 500 patients reported that 14 (2.8%) of these patients had a positive patch test initially, but only 2 (0.4%) had a true allergy to PI with a subsequent positive repeat open application test (ROAT) (21). IgE-mediated anaphylactic reactions to PI are rare, with fewer than ten cases reported in the literature. In patients with a documented allergy to PI, it is essential to take a thorough history to rule out an allergy to iodine or iodine-containing substances as the cause. Suppose concerns over PI allergy remain after patch testing and confirmatory testing may be performed in cases where it is appropriate to delay treatment (2). For rare cases of a confirmed true PI allergy, aqueous chlorhexidine 0.05% may be used as an alternative (5). In most cases, however, PI can be safely administered, and its essential role in preventing post-operative and post-IVI endophthalmitis far outweighs its risk of irritant reactions.
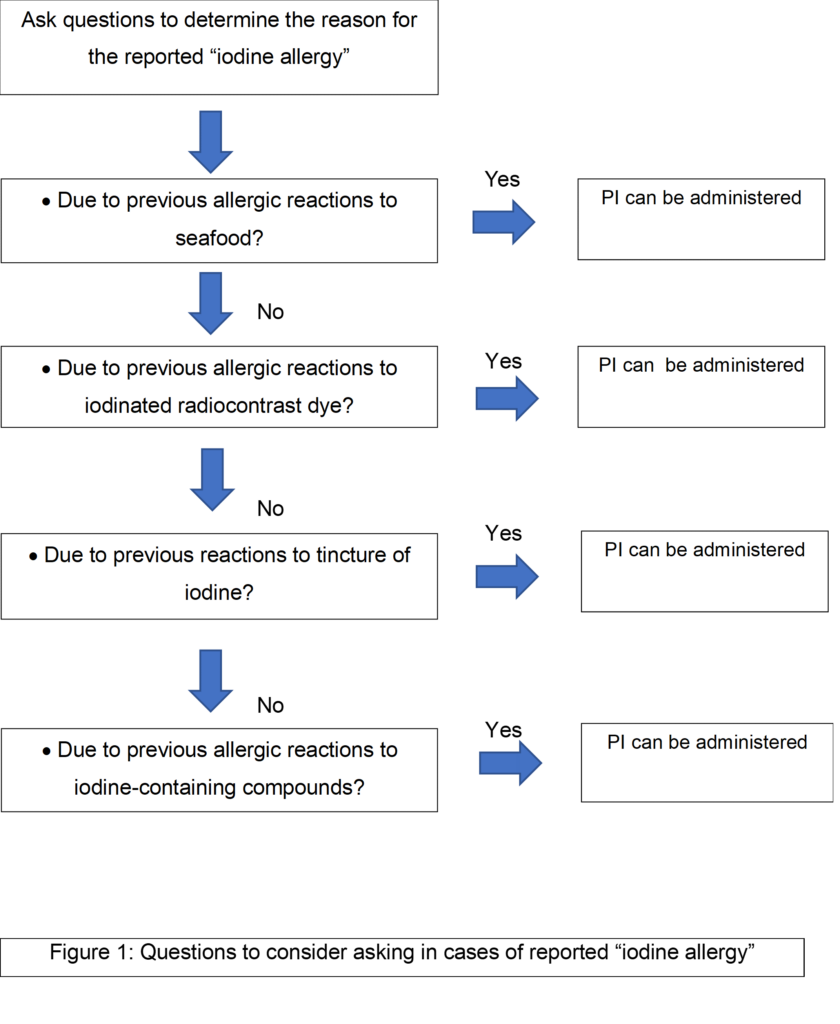
Approach to Cases of Reported “Iodine Allergy”
When patients voice concerns about ‘iodine allergy’, we propose administration of a set of questions to determine the true nature of the past event that the patient links with ‘iodine allergy’. (Fig 1). We consider it is safe to administer PI to patients who answer ‘yes’ to the questions listed.
Conclusion
PI is an essential agent for preventing endophthalmitis after ocular surgeries and intravitreal injections. In cases where patients voice concerns before administration, it is helpful to consider asking the above questions and carry out additional allergy testing to confirm a true allergy to PI. [i]This would help to ensure that PI is administered appropriately to reduce the risk of ocular morbidity.
References
- Nentwich MM, Ta CN, Kreutzer TC, Li B, Schwarzbach F, Yactayo-Miranda YM, et al. Incidence of postoperative endophthalmitis from 1990 to 2009 using povidone-iodine but no intracameral antibiotics at a single academic institution. J Cataract Refract Surg 41(1), 58-66 (2015)
- Modjtahedi BS, van Zyl T, Pandya HK, Leonard RE 2nd, Eliott D. Endophthalmitis After Intravitreal Injections in Patients With Self-reported Iodine Allergy. Am J Ophthalmol 170, 68-74 (2016)
- Mulcahy LT, Schimansky S, Fletcher E, Mohamed Q. Post-injection endophthalmitis rates with reduced povidone-iodine prevention in patients with self-reported iodine sensitivity. Eye (Lond) 35(6), 1651-1658 (2021)
- Durani P, Leaper D. Povidone-iodine: use in hand disinfection, skin preparation and antiseptic irrigation. Int Wound J 5(3), 376-87 (2008)
- Barry P, Cordovés L, Gardner S. ESCRS Guidelines for Prevention and Treatment of Endophthalmitis Following Cataract Surgery: Data, Dilemmas and Conclusions. Ireland: European Society of Cataract and Refractive Surgeons; 2013. https://www.escrs.org/media/uljgvpn1/english_2018_updated.pdf [Accessed 24th July 2023].
- Patel AS, Benson CE, Masters JS, DelMonte DW, Kourtney H. Povidone-Iodine in Ophthalmic Surgery. 2023. https://eyewiki.aao.org/Povidone-Iodine_in_Ophthalmic_Surgery#:~:text=Despite%20the%20wide%2Dspread%20use,of%20endophthalmitis%20after%20intraocular%20surgeries.
- Hinkle JW, Wykoff CC, Lim JI, Hahn P, Kim SJ, Tabandeh H, et al. “Iodine Allergy” and the Use of Povidone Iodine for Endophthalmitis Prophylaxis. J Vitreoretin Dis 4(1), 65-68 (2019)
- Stewart MW. Doctor I Have an Iodine Allergy. Ophthalmol Ther 11(3), 931-938 (2022)
- Bellchambers AS, Wearne MJ. Intraocular surgery endophthalmitis prophylaxis with self-reported iodine allergy. J Cataract Refract Surg 46(5), 795-796 (2020)
- Institute for Quality and Efficiency in Health Care (IQWiG). Allergies: Overview. 2016. https://www.ncbi.nlm.nih.gov/books/NBK447112/ [Accessed July 2023]
- Tanno LK, Calderon MA, Smith HE, Sanchez-Borges M, Sheikh A, Demoly P, et al. Dissemination of definitions and concepts of allergic and hypersensitivity conditions. World Allergy Organ J 9:24 (2016)
- Douglass JA, O’Hehir RE. Diagnosis, treatment and prevention of allergic disease: the basics. Med J Aust 185(4), 228-33 (2006)
- Johnston RB Jr, Branch S, Brent G, Brown R, et al. Health Implications of Perchlorate Ingestion. Washington: National Academies Press; 2005. https://doi.org/10.17226/11202. [Accessed 24th July 2023]
- National Health Service. Iodine: vitamins and minerals. 2020. https://www.nhs.uk/conditions/vitamins-and-minerals/iodine/#:~:text=How%20much%20iodine%20do%20I,a%20varied%20and%20balanced%20diet.
- Zimmermann MB. Iodine Deficiency. Endocr Rev 30(4), 376-408 (2009)
- National Institutes of Health. Iodine. 2022. https://ods.od.nih.gov/factsheets/Iodine-Consumer/.
- Wykoff CC, Flynn HW Jr, Han DP. Allergy to povidone-iodine and cephalosporins: the clinical dilemma in ophthalmic use. Am J Ophthalmol. 151(1), 4-6 (2011)
- Lopata AL, Kleine-Tebbe J, Kamath SD. Allergens and molecular diagnostics of shellfish allergy: Part 22 of the Series Molecular Allergology. Allergo J Int 25(7), 210-218 (2016)
- Wulf NR, Schmitz J, Choi A, Kapusnik-Uner J. Iodine allergy: Common misperceptions. Am J Health Syst Pharm 78(9), 781-793 (2021)
- Schabelman E, Witting M. The relationship of radiocontrast, iodine, and seafood allergies: a medical myth exposed. J Emerg Med 39(5), 701-7 (2010)
- Lachapelle JM. Allergic contact dermatitis from povidone-iodine: a re-evaluation study. Contact Dermatitis 52(1), 9-10 (2005)
