Diya Baker
Birmingham Midlands Eye CentreRishika Chaudhary
Birmingham Midlands Eye CentreHamza Duffaydar
University of Birmingham Medical SchoolKim Lett
Birmingham Midlands Eye Centre
Summary
A case of a 21-year-old male attending eye casualty with left eye pain and blurred vision for 5 days and associated with a sudden onset headache. The patient had a history of homocystinuria that was medically managed. The patient had no significant social history. Significant findings on examination included left eye intraocular pressure (IOP) 67mmHg, best corrected visual acuity (BCVA) 1/60, left corneal oedema and left lens dislocation into the anterior chamber. Following medical management, the patient underwent cyclodiode laser of the left eye. On follow up, the patient symptomatically improved however examination revealed conjunctival hyperaemia and bilateral ectopia.
A fortnight following, the patient experienced severe right ocular pain and had IOP of 60mmHg. The patient underwent right eye cyclodiode laser, lens extraction, capsular tension ring, automated anterior vitrectomy and IOL insertion.
Background
Homocystinuria is an inherited metabolic disorder characterised by mutations in the cystathionine beta synthase gene. As a result, the body is unable to metabolise the amino acid homocysteine, an important molecule in several metabolic processes.[1] The condition has two clinical phenotypes; a milder pyridoxine (Vitamin B6) responsive form and a more severe pyridoxine non-responsive form. The management of the former subset is predominantly pyridoxine supplementation whilst that of the latter is a methionine restricted diet.[2] The global incidence of pyridoxine-resistant homocystinuria is estimated at 1 in 200 000 to 1 in 335 000 although the disorder is more common in certain countries such as Ireland where incidence is 1 in 65 000 people.[3] In the United Kingdom, babies undergo a heel prick test to screen for homocystinuria along with eight other rare but serious conditions, as part of the National Bloodspot Screening programme.[4] This is because if recognised early and treated appropriately patients may lead a normal life. Left untreated, almost a quarter of patients are likely to die before the age of 30 from a thromboembolic event.[1]
Case Presentation
A 21-year-old male with a known history of homocystinuria and bilateral lens dislocation presented to the Ophthalmic Emergency department of a tertiary eye centre. He reported a 5 day history of pain and blurred vision in his left eye (LE) with a sudden onset diffuse headache lasting a day. The patient’s regular prescribed medications included pyridoxine 30mg od PO and folic acid 5mg od PO although he admitted having poor compliance due to his work as a forklift driver.
On examination visual acuity (VA) was 1/60 in the LE and 6/12 in the right eye (RE). Intraocular pressures (IOP) were LE 67mmHg and 15mmHg RE. The LE cornea was mildly oedematous with the LE lens displaced into the anterior chamber (AC). Examination of the RE showed the lens in the posterior chamber (PC).
Treatment
The patient was commenced on g. dexamethasone 0.1% QDS and intravenous (IV) acetazolamide 500mg. He was positioned supine and given analgesia. After 1 hour, the LE IOP had reduced to 56mmHg and g. Cosopt bd, g. iopidine 1% tid, g. pilocarpine 2% tid and IV mannitol 1g/kg was added. Subsequently his LE IOP dropped to 36mmHg and he remained comfortable overnight. The following morning, he was awoken by worsening LE pain and nausea. The LE IOP had risen again to 50mmHg and on examination the LE lens remained in the AC with endothelial touch and corneal oedema.
Topical mydriatics were commenced: g. cyclopentolate 1% qid, g, tropicamide 1% qid and g. phenylephrine 1% qid. The patient was positioned supine, enabling the lens to drop back into the PC [Figure 1]. The patient underwent emergency cyclodiode laser treatment between 3-9 o’clock (180°) and received further IV acetazolamide 500mg and 20% IV Mannitol. Post-operatively the patient continued supine posturing with g. pilocarpine 2% qid. After 36 hours observation, the LE lens had fully repositioned into the PC [Figure 2].
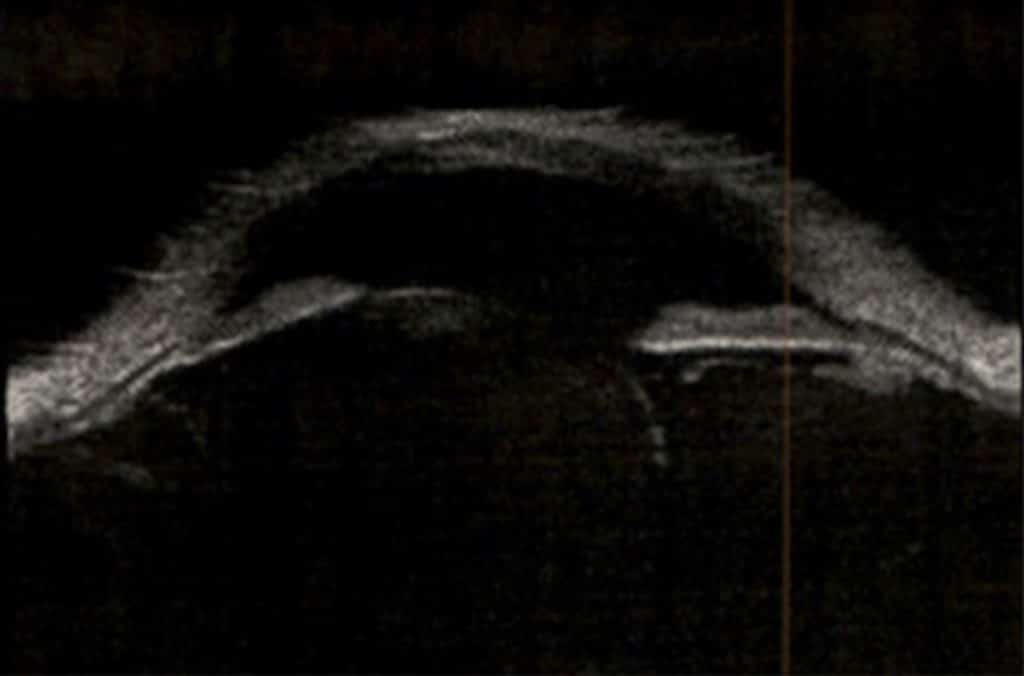
Figure 1 USS of left lens dislocation in posterior chamber following topical mydriatics and supine positioning. 
Figure 2 USS of left lens dislocation in posterior chamber 36 hours following emergency cyclodiode laser treatment.
Outcome
At three-week follow-up, the patient reported an improvement of blurred vision and pain in the LE. LE VA was 6/60 and IOP was 14mmHg. Examination demonstrated LE mild conjunctival hyperaemia, clear cornea and bilateral ectopia lentis. The patient agreed to elective LE lens extraction and implantation of an intraocular lens.
Two weeks later the patient re-attended the emergency department, this time for a one-day history of severe pain in his right eye and vomiting. VA of the RE was 6/36 and there was conjunctival hyperaemia noted. The RE lens was displaced into the AC and RE IOP was 60mmHg. He again admitted to poor medication compliance and was admitted to the ophthalmic ward. The patient was treated with the same pharmacological regime as described previously and his RE IOP reduced to 20mmHg. The following day he underwent RE cyclodiode laser therapy along with lens extraction, capsular tension ring (CTR), automated anterior vitrectomy and intra-ocular lens insertion. Post-operatively the patient was given pilocarpine and his IOP remained stable bilaterally at 10mmHg. His visual acuity was 6/18 in his right eye and 6/36 in his left eye. Six days later he required subconjunctival injection of dexamethasone 4mg for post-operative inflammation. The patient is due to undergo a similar operation to his LE as previously scheduled.
Discussion
The major clinical manifestations of patients with homocystinuria are a result of the elevated plasma homocysteine level. These may include ectopia lentis and skeletal deformities as a result of sulfhydryl groups of homocysteine interfering with collagen cross-linkages. Further clinical manifestations include thrombosis and widespread arterial and venous occlusions at a young age due to platelet dysfunction.[5] In patients with homocystinuria, subluxation of the lens typically occurs bilaterally, symmetrically and at an inferonasal position. It is the most common sign leading to the diagnosis of the condition and occurs at a relatively young age in children.[1] In a study by Mudd et al,[1] 86% of participants were diagnosed on the basis of ectopia lentis, of which 50% of patients with the pyridoxine resistant form had by the age of 6 and 50% of patients with the pyridoxine responsive form had by the age of 10. A lack of zonular integrity due to enzyme defect has been thought to be the cause for lens displacement.[5] Other ocular manifestations include retinal degeneration, cataracts and secondary glaucoma as experienced by this patient.[6] The condition is also associated with progressive myopia. This may be due to spherical deformation of the lens, spherophakia, as a result of degenerating zonular fibres which normally control the shape of the lens. As lens subluxation progresses, the patient may develop further astigmatism. The literature has shown a positive correlation between lens subluxation and increased ocular axial length with homocystinuria patients who experience complete lens dislocation having significantly increased ocular axial length.[7] However, by the age of 10, axial length of the eyes remains fixed and thus homocystinuria patients who have adhered to treatment until that age will have minimal myopic astigmatism.[8]
Acute angle closure glaucoma can commonly occur with lens dislocation as the lens may displace into the anterior chamber and obstruct outflow of aqueous humour causing raised intraocular pressure.[9] Management is through a combination of drugs including steroids, carbonic anhydrase inhibitors, beta blockers, acetazolamide, mannitol and pilocarpine to reduce intraocular pressure and inflammation. Further treatment then involves laser iridotomy.[10] However, the definitive treatment for ectopia lentis in homocystinuria patients remains cataract extraction stabilised by capsular tension ring and insertion of an artificial lens. An evaluation study by Yaguchi et al. demonstrated the benefits of using capsular tension ring (CTRs) and how they can facilitate phacoemulsification, aspiration and intraocular lens aspiration. CTRs increase the capsule equatorial diameter and support areas of zonular dehiscence by redistributing zonular tension around the capsule.[11] As a consequence the intraocular lens’s near planar face, increased zonular diameter, minimal axial length and posterior vault reduce the likelihood of recurrent transpupillary movement.
This case also highlights the need for consideration of bilateral surgery in patients with bilateral zonular pathology and poor compliance with medications, to avoid further complications arising in the time interval between the surgeries. Furthermore, there is the added benefit of the patients only undergoing one episode of general anaesthesia which is of significance especially given that patients with homocystinuria are at an increased risk of general anaesthetic complications including thromboembolism, pneumothoraces and severe hypertension due to infarction.[12] Whilst currently there is no literature comparing unilateral against bilateral ocular surgery for homocystinuria patients specifically, bilateral surgery could have a potential to be safer for patients both from an ophthalmic and anaesthetic perspective.
Learning Points
- Acute angle closure is a sight-threatening condition; consideration of secondary causes as well as early recognition is key and management via immediate referral to Ophthalmology is vital.
- This case highlights the challenges of management of lens dislocation in patients with homocystinuria. Management of lens dislocation is initially with pupillary dilation and medical management of raised IOP, supine posturing and then pupillary constriction when the lens repositions into the retropupillary space.
- The need for meticulously planned bilateral ophthalmic surgery; in this case the subsequent post-operative complications highlight the importance of regular and thorough monitoring post operatively.
- The presence of bilateral zonular pathology, particularly in the case of poor patient medication compliance, should prompt consideration of planned (possibly immediate) sequential bilateral surgery.
References
- Mudd SH, Finkelstein JD, Irreverre F, Laster L. Homocystinuria: An Enzymatic Defect. Science 1964;143(3613):1443-1445.
- Morris AAM, Kožich V, Santra S, Andria G, Ben-Omran T, Chakrapani AB, et al. Guidelines for the diagnosis and management of cystathionine beta-synthase deficiency. J Inherit Metab Dis 2016;40(1):49-74.
- Homocystinuria [Internet]. Genetics Home Reference. 2020 [cited 27 September 2020]. Available from: https://ghr.nlm.nih.gov/condition/homocystinuria#statistics
- Newborn blood spot screening: programme overview [Internet]. GOV.UK. 2020 [cited 27 September 2020]. Available from: https://www.gov.uk/guidance/newborn-blood-spot-screening-programme-overview
- Grieco AJ. Homocystinuria: pathogenetic mechanisms. Am J Med Sci. 1977 Mar-Apr;273(2):120-32.
- Martínez-Gutiérrez J,D., Mencía-Gutiérrez E, Gracia-García-Miguel T, Gutiérrez-Díaz E, López-Tizón E. Classical familial homocystinuria in an adult presenting as an isolated lens subluxation. Int Ophthalmol 2011;31(3):227-232.
- Mulvihill A, O’Keeffe M, Yap S, Naughten E, Howard P, Lanigan B. Ocular axial length in homocystinuria patients with and without ocular changes: effects of early treatment and biochemical control. J AAPOS. 2004 Jun;8(3):254-8. doi: 10.1016/j.jaapos.2004.01.010.
- Gordon RA, Donzis PB. Refractive development of the human eye. Arch Ophthalmol. 1985 Jun;103(6):785-9. doi: 10.1001/archopht.1985.01050060045020.
- Harrison DA, Mullaney PB, Mesfer SA, Awad AH, Dhindsa H. Management of ophthalmic complications of homocystinuria. Ophthalmology 1998;105(10):1886-1890.
- Murray D. Emergency management: angle-closure glaucoma. Community eye health 2018;31(103):64.
- Yaguchi S, Yaguchi S, Bissen-Miyajima H. Evaluation of Lens Capsule Stability Using Capsular Tension Ring, Iris Retractor, and Capsule Expander Using a Porcine Model With Zonular Dehiscence. Invest Ophthalmol Vis Sci 2019;60(10):3507.
- Upadhay SP, Rajmohan N. Anesthetic implications of homcystinuria: A case report. Journal of Anaesthesia and Critical Care Case Reports Jan- Apr 2018; 4(1):12-15.
