Madiah Mahmood
Teaching and placement opportunities within ophthalmology vary across UK medical schools and the foundation programme. Ophthalmic pathology can present in various settings, such as acutely in the emergency department, in general practice, and among inpatients where patients may develop an ocular complaint or an ophthalmic manifestation of systemic disease (1). It is therefore important to develop a strong foundational knowledge of this speciality (1). The GMC state “good medical practice” incorporates providing good clinical care including but not exclusive to the following domains: (2)
- Adequately assess history / symptoms
- Relevant psychological, spiritual, social, economic and cultural factors
- The patient’s views, needs and values
- Carry out physical examination where required
- Propose, provide or prescribe/arrange suitable investigation or treatment where necessary
This article aims to highlight several common ophthalmic presentations, providing valuable support for your medical school final exam preparation and as preparation as you begin your foundation year as a resident doctor. Guidance on which conditions are relevant for your learning has been sought from The Royal College of Ophthalmologists (3). Section 2 includes a short quiz designed to help you recognise how cases may appear in an exam setting or how patients might present clinically. Answers are provided at the end of each question.
1. The Red Eye
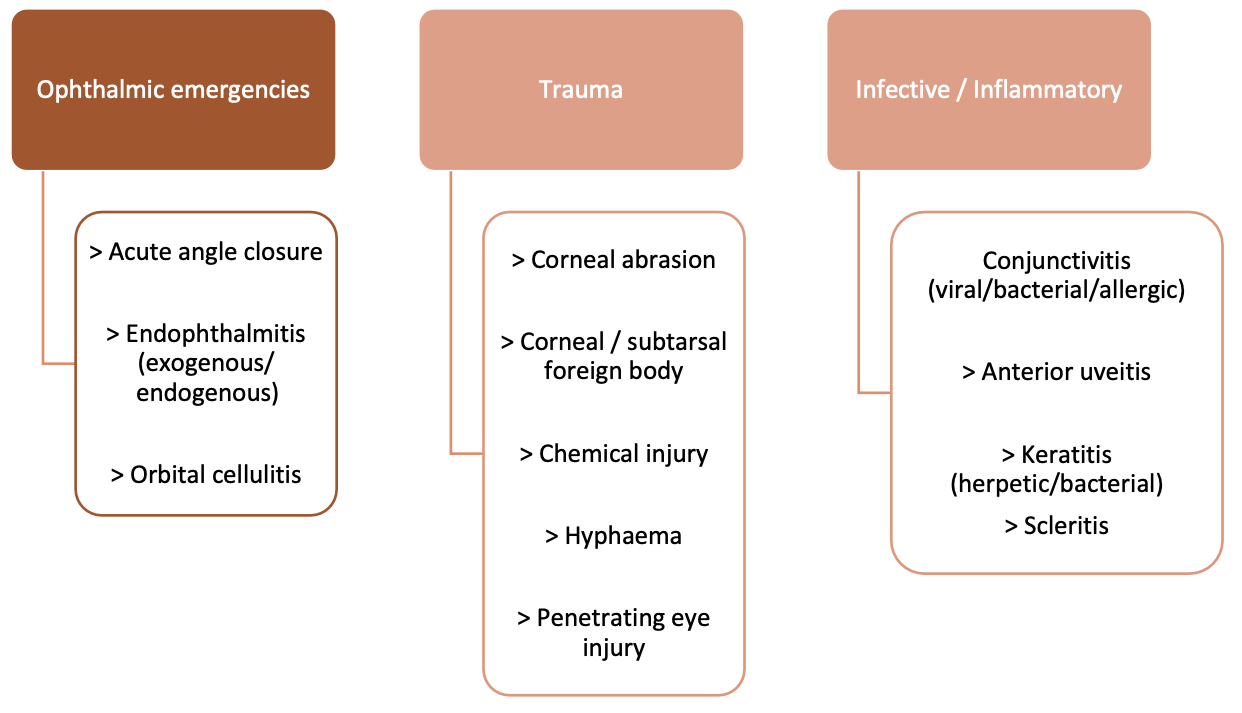
Note: Hyphaema and penetrating eye injuries do not always present with a red eye Chemical injuries can be considered ophthalmic emergencies and may present unexpectedly white in extreme injury due to ischaemia
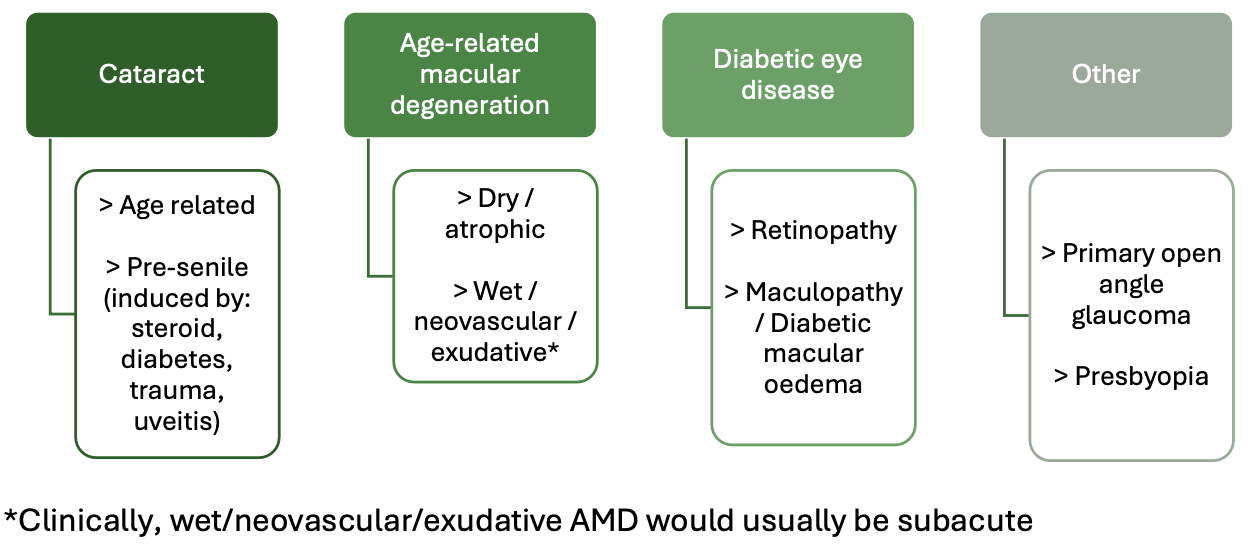
2. Gradual Vision Deterioration
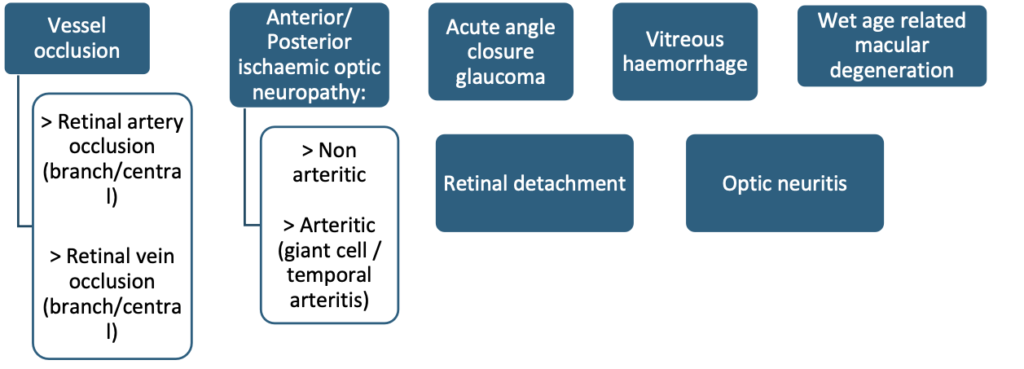
3. Sudden or Subacute Vision Loss
Sudden vision loss is an emergency – refer to ophthalmology services urgently
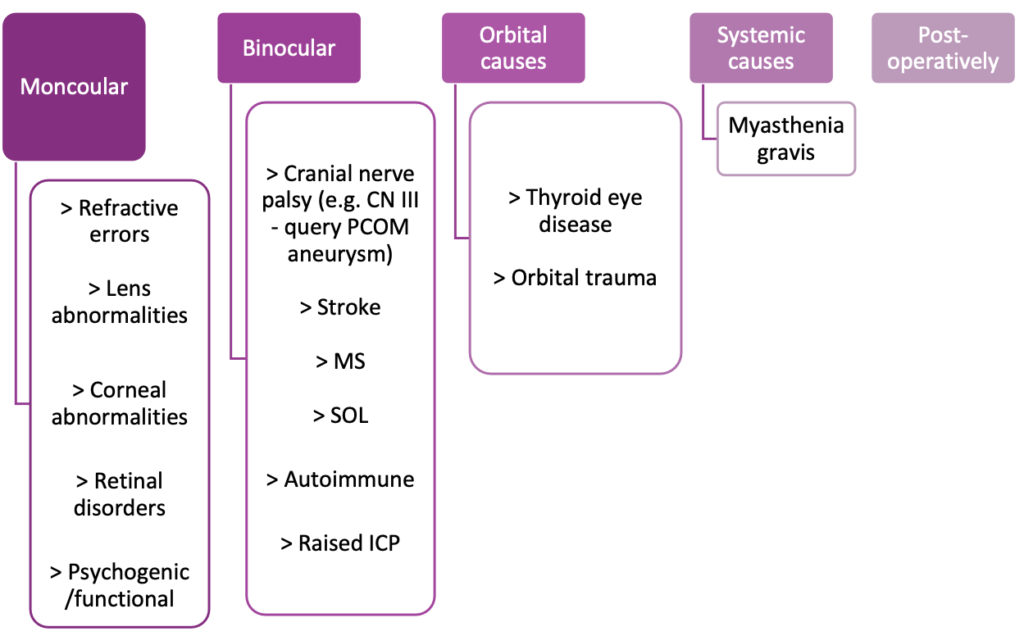
4. Diplopia
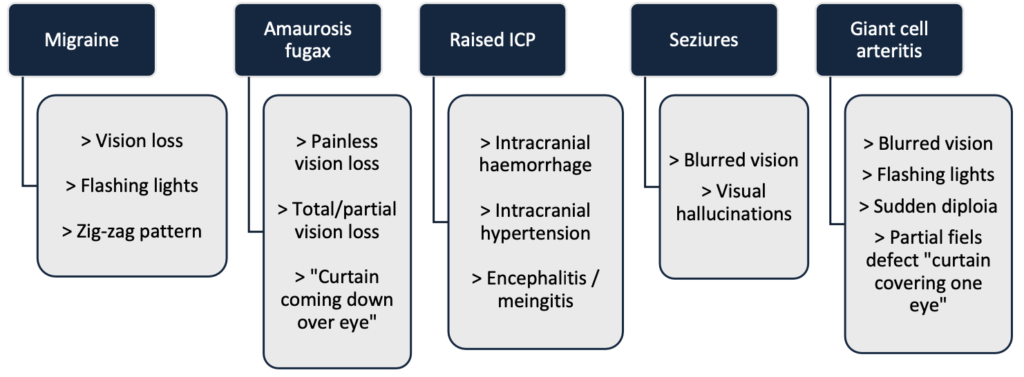
5. Transient Visual Symptoms
6. Other Common Diagnoses
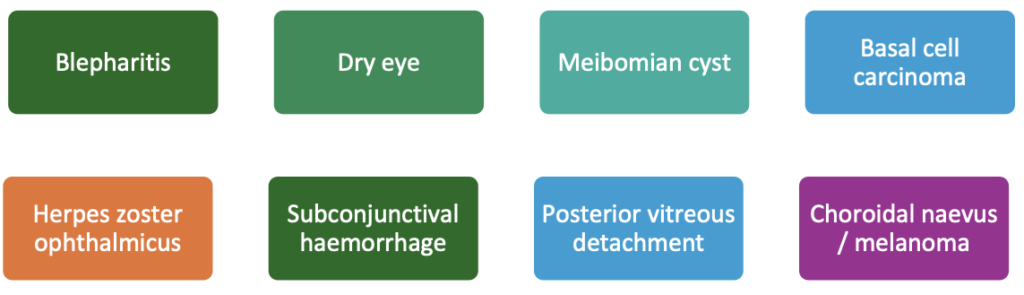
The Royal College of Ophthalmologists indicate medical students should be able to define and identify the causes and management the following conditions:
- Ambylopia
- Myopia and hyperopia
- The normal colour, cupping and contour of the optic disc and causes of abnormalities.
Section 2
1) A 55-year-old female presents to the emergency department with extreme right eye pain which has lasted for 5 hours. She denies changes to her vision, nausea or vomiting and has a past medical history of rheumatoid arthritis for which she takes methotrexate. Her observations are stable. The right eye is red and when palpated through her closed lids the eye is tender to touch. There are no abnormalities with the left eye.
What is the most likely diagnosis?
- Episcleritis
- Scleritis
- Conjunctivitis
- Keratitis
Answer: b) Scleritis – a cause of red eye which is often very painful, waking the patient from sleep and can present with blurred vision. Connective tissue diseases are often associated with scleritis. Phenylephrine drops can help differentiate between scleritis and episcleritis – if eye redness improves then the diagnosis will be episcleritis as it blanches conjunctivital and episcleral vessels but does not blanch scleral vessels.
2) A 33-year-old female presents to the GP with increasingly blurred vision in her right eye over the past week. She experiences pain on eye movement and feels colours appear washed out compared to the left eye. Vision in the left eye appears normal. She has been feeling lethargic for the past month but feels this is likely due to entering the winter months and it is getting darker and colder, making her feel “less energised”.
What is the most likely diagnosis?
- Retinal detachment
- Episcleritis
- Retinal Detachment
- Temporal arteritis
- Optic neuritis
Answer: e) Optic neuritis – this patient has symptoms of typical optic neuritis: Reduced visual acuity, reduced colour vision, pain on eye movements. There may also be a central scotoma on visual field testing. The diagnosis can be confirmed with an MRI brain and orbits with gadolinium and lumbar puncture. This may show cortical white matter changes if the patient has multiple sclerosis which is a common association.
3) A 14-year-old male visits the GP due to a red, painful watering right eye for 5 days. He states his left eye is now also starting to water. He has found it irritating and been rubbing it a lot. He denies visual changes but said he woke up with thick, green discharge in the eye making his right-sided eyelashes sticky. His right eye appears injected throughout and you can see some discharge in the inner corner of the eye. He has no other past medical history and is worried his eye problem will impact his football training this Saturday.
Given the most likely diagnosis, what is the first line treatment?
- Oral amoxicillin
- Steroid eye drops
- Chloramphenicol ointment
- Hot compress
Answer: c) Chloramphenicol ointment. The patient likely has bacterial infective conjunctivitis. Generally, viral conjunctivitis is a self-limiting condition whereby discharge symptoms can be eased by cleaning with a warm compress and itching/rubbing can be relieved with a cold compress. However, chloramphenicol is often offered to alleviate severe presentation in bacterial conjunctivitis A swab should be sent if there is a significant amount of discharge. NICE recommend: “Treat with topical antibiotics if severe or circumstances require rapid resolution”. Note in pregnant patients fusidic acid should be offered instead.
References
- The Royal College of Ophthalmologists. 2023. Medical Students & Foundation Doctors. [Online]. [DOA 20/11/24]. Available from:https://www.rcophth.ac.uk/our-work/ophthalmology-careers/medical-students-and-foundation-doctors/
- General Medical Council. 2024. Good medical practice Domain 1: Knowledge, skills and development. [Online]. [DOA 20/11/24]. Available from:https://www.gmc-uk.org/professional-standards/the-professional-standards/good-medical-practice/domain-1-knowledge–skills-and-development#being-competent-7635AD7E6015468795D857F3F1FBC92D
- The Royal College of Ophthalmologists. 2022. Education and Training Department 2020 RCOphth Curriculum for Undergraduates and Foundation Doctors. [Online]. DOA [20/11/204]. Available from:https://www.rcophth.ac.uk/wp-content/uploads/2022/03/Curriculum-UG-RCOphth-220309.pdf
