Raheel Faiz1, Samer Elsherbiny1
1Ophthalmology Department, South Warwickshire NHS Foundation Trust
Comorbidity among ophthalmology patients is under recognised. Patients often need to see multiple sub-specialists for multiple conditions, and this can be overwhelming and often leads to appointments being missed. This is because currently there is a mismatch between the capacity and demand that current NHS Ophthalmology departments can offer. It was reported that 630,000 patients were waiting for an ophthalmology appointment in 2023 in comparison to 260,000 in 2011 (1).
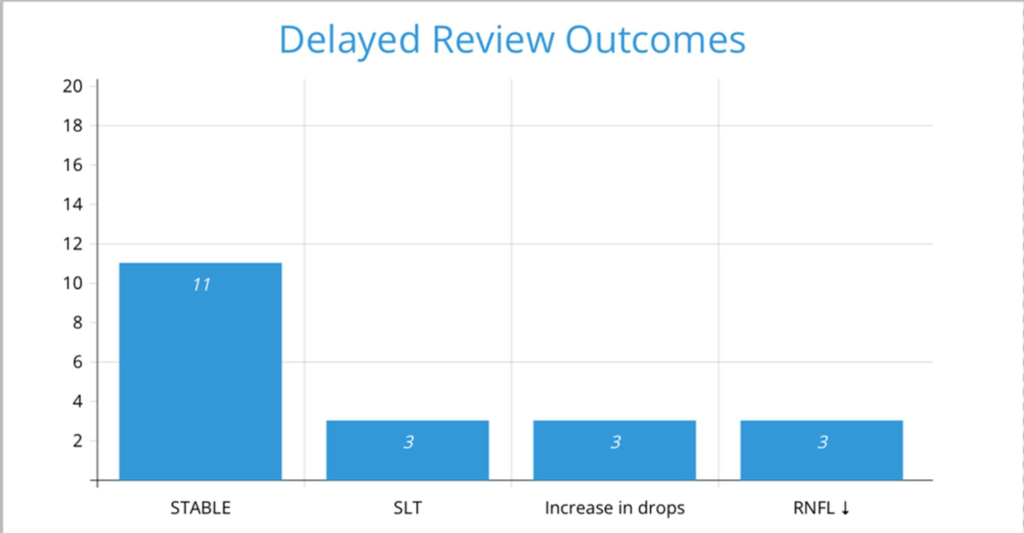
It was noted in our unit that approximately 12% of patients attending medical retina clinics were also due to be monitored in the glaucoma clinic. Many were noted to be overdue their glaucoma review with little or no mention of this in the multiple, consecutive medical retina reviews. Moreover, many of the patients thought they were being assessed for all their eye conditions at any given visit. We audited whether patients with both medical retinal pathologies and glaucoma/ocular hypertension received timely glaucoma monitoring according to NICE guidelines for glaucoma monitoring. The audit included 50 patients seen between July 2023 and January 2024 at South Warwickshire University NHS Foundation Trust. Data on demographics, clinical history, diagnoses, and management plans were extracted from Medisoft (the electronic patient record system). Condition progression for glaucoma was defined as either treatment escalation or visual field loss determined by perimetry analysis at the subsequent visit to the glaucoma clinic (having been flagged by this audit). The data revealed that among 50 overdue patients in the glaucoma clinic, 32 had glaucoma and 18 had ocular hypertension. After analysing their appointments, data was available for 20 patients’ post-review. Of these, 11 (55%) were stable, while three (15%) required selective laser trabeculoplasty (SLT) in addition to their current medication, another three (15%) needed an increase in anti-glaucoma drops, and three (15%) experienced vision deterioration or thinning of the retinal nerve fibre layer (RNFL) that did not necessitate new treatment due to compliance issues. The remaining 30 patients had not yet been seen in the glaucoma clinic.

Our data highlights patient factors and service factors that pose a risk to the patients’ vision. Patient factors include the level of understanding patients have regarding their multiple eye conditions. Many patients are unaware of the extent of specialist care, even in small eye units. This issue is particularly concerning for conditions like glaucoma, where vision loss is gradual and insidious. The problem is compounded by the fact that these issues are more common in older patients, who may find it overwhelming to manage multiple appointments due to the greater probability of medical comorbidities, travelling difficulties and cognitive decline which often makes them dependant on a family member for medical visits (2).
‘’POAG affects about 1% of people aged 40, about 3% of people aged 60, and about 8% of people aged 80 years’’ (3). According to the Royal College of Ophthalmologists “permanent harm from delays to care, in terms of avoidable visual loss, is 9 times more likely to happen in follow-up patients than in new patients” (4). Service factors include education and training for all medical and non-medical members of the increasingly multi-disciplinary team carrying out clinical duties in the current model of service delivery. This includes the booking and administrative staff (5). Getting it right first time (GIRFT) (a national programme that aims to try to improve the efficiency and reduce variability of eye units) proposes appointing a failsafe officer responsible for ensuring local ophthalmology departments meet targets for timely interventions, patient follow-ups, and escalating overdue appointments. The imperative to see new patients may be a risk factor delaying follow-up appointments.
Measures taken to address this risk include video or telephone consultations which have become more widespread since Covid-19. This does not necessarily address other factors affecting attendance for the diagnostic tests nor the need to attend different subspecialty clinics. Tong et al. carried out a study to determine factors that contributed to missed follow up appointments in an outpatient setting (6). They demonstrated that greater distance between home and clinic was positively associated with loss to follow-up.
Locally, we have implemented the use of customisable flagging of relevant issues on the EPR (Medisight) to highlight patients who have an “eye co-morbidity”. This is a readily visible icon on the “home screen” of a given patient’s record. The training carried out locally in August 2024 was to promote the use of this icon (especially in the absence of a glaucoma failsafe officer) to alert staff seeing patients in the medical retina clinic to ensure they review the entirety of the patient’s record for all of their eye conditions and to confirm the patient understands what other eye conditions they have to be seen for. This is consolidated by appropriate documentation in the EPR and requesting the outstanding appointment to be booked.
One month after the initial presentation of this audit and following the training on the implementation of the flag on the EPR, patients’ records were reviewed from the medical retina clinic who were also diagnosed with glaucoma/ocular hypertension in addition to their medical retina condition. The purpose was to assess two metrics. First, how many patients’ records had the flag signifying ocular comorbidity. Second, how many records had documentation by the medical retina staff member seeing the patient stating they have verified when the next glaucoma review is with the patient and, if not booked, documenting it was requested.
382 patient records that met the selection criteria from 1st September 2024 to 31st October 2024 were reviewed. 324 (85%) had the flag; 173 (45%) had documentation verifying when the next glaucoma appointment review is; 209 (55%) stated the glaucoma appointment was not booked and has been requested.
Unlike systemic comorbidity, ocular comorbidity is much less appreciated and there is less data available in terms of its potential impact on patients (7). This is due to patient and service factors. EPR alerts, remote clinics, and sharing workloads across a trained multi-disciplinary team can help reduce vision loss risks caused by current service capacity and staff awareness limitations.
References
- Association of Optometrists. Tackling the hospital outpatient backlog in eye care [Internet]. London: Association of Optometrists; 2023 Mar 21 [Accessed 04 September 2024]. Available from: https://www.aop.org.uk/our-voice/policy/position-statements/2023/03/21/tackling-the-hospital-outpatient-backlog-in-eye-care
- Moustafa GA, Borkar DS, Eton EA, Koulisis N, Kloek CE; PCIOL Study Group Members. Healthcare disparities contribute to missed follow-up visits after cataract surgery in the USA: results from the perioperative care for intraocular lens study. BMJ Open. 2021;11(3)
- National Institute for Health and Care Excellence (NICE). Glaucoma: Background Information – Prevalence [Internet]. London: NICE; 2017 [Accessed 04 September 2024]. Available from: https://cks.nice.org.uk/topics/glaucoma/background-information/prevalence/
- Marshall J. Scale of ophthalmology follow-up backlogs and need for better data collection highlighted by thinktank [Internet]. London: The Royal College of Ophthalmologists; 2023 Oct 31 [Accessed 4th September 2024]. Available from: https://www.rcophth.ac.uk/news-views/scale-of-ophthalmology-follow-up-backlogs-and-need-for-better-data-collection-highlighted-by-thinktank/
- MacEwen C, Davis A, Chang L. Ophthalmology GIRFT Programme National Specialty Report [Internet]. London: Getting It Right First Time; 2019 Dec [Accessed 06 September 2024]. Available from: https://gettingitrightfirsttime.co.uk/wp-content/uploads/2019/12/OphthalmologyReportGIRFT19P-FINAL.pdf
- Michelle TCY, Victoria KRY, Eng Sing L. A scoping review on the factors associated with the lost to follow-up (LTFU) amongst patients with chronic disease in ambulatory care of high-income countries (HIC). BMC Health Serv Res. 2023;23:883
- Griffith JF, Goldberg JL. Prevalence of comorbid retinal disease in patients with glaucoma at an academic medical center. Clin Ophthalmol. 2015;9:1275–1284.
