Hamzah Hussain, Ahmed Javed
This case report follows the case of a 27 year old female who presented to her optometrist with a 10-day history of floaters in her left eye. The optometrist noted papilloedema and she was advised to attend the Emergency Department for further assessment and imaging. A CT brain showed no acute intracranial findings, however upon examination a left swollen disc was noted and the right pupil was unreactive to light. She was referred to eye casualty for specialist input. Her visual acuity was 0.16 in her right eye and 0.42 in her left eye. Ishihara plates could be read fully. Pupillary reflexes were normal in the left eye however the patient reported that the right eye has been unreactive since birth. Further examination findings included; normal ocular movements bilaterally with no proptosis, both anterior segments were normal. In the right eye congenital corectopia was noted with iris atrophy and a fibrovascular membrane. At the same time, macula granularity as well as a subtle chalky white spot lesion were spotted in the left eye. The images can be seen in the figures below as well as an OCT which was done.


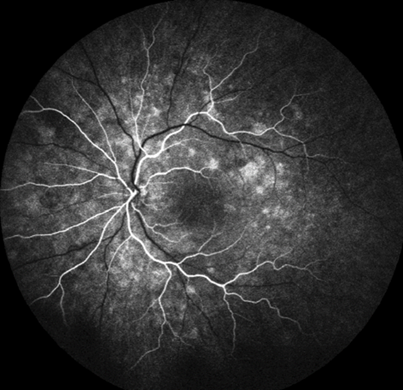
This type of presentation is uncommon and therefore the information was required to be amalgamated in order to diagnose the patient. Firstly, white-dot syndromes are typically bilateral except for Multiple Evanescent White Dot Syndrome (MEWDS). The focal granularity also supported this diagnosis. The papilloedema may have been misleading in this case, but this is unusual in optic neuropathy and nerve function was intact. The diagnosis was therefore likely to be MEWDS and the patient was suitable for an FFA. This can be seen in figure 4 below.
In the follow up clinic, the symptoms had resolved but there was a remaining blind spot from the optic disc swelling which was resolving. The patient was discharged with safety-netting.
Discussion
MEWDS is a rare condition itself, affecting mainly the outer retina. The exact aetiology of MEWDS is unknown however there seems to be an association with a viral prodrome (1). Symptoms typically include; unilateral blurry vision, visual field loss and floaters. It should be considered as a differential in any middle-aged female presenting with these symptoms as it affects females roughly four times more than men (2). Multi-modal imaging can help to distinguish MEWDS from other white-dot syndromes and these include Fluorescein angiography (FFA) and optical coherence tomography (OCT). Some of the characteristic findings of MEWDS can be seen in the figures including foveal granularity and hyperfluorescence. Visual prognosis is typically very good, as MEWDS is a self-limiting condition – however recurrence can occur in up to 10% of patients (2). It must be noted that more sinister conditions have been known to masquerade as MEWDS including sarcoidosis (3) and therefore if investigations point away from the diagnosis, more serious conditions should be excluded.
Learning points
- MEWDS should be considered a differential in healthy middle-aged females (20-50 yrs old) who present with acute onset, painless visual disturbances.
- Multi-modal imaging may be necessary to confirm the diagnosis.
- No treatment is usually required and prognosis is excellent.
References
- Goldman, D. and Muakkassa, N., 2018. Multiple Evanescent White Dot Syndrome. Atlas of Retinal OCT: Optical Coherence Tomography, pp.107-108.
- Eyewiki.aao.org. 2022. Multiple Evanescent White Dot Syndrome – EyeWiki. [online] Available at: <https://eyewiki.aao.org/Multiple_Evanescent_White_Dot_Syndrome> [Accessed 30 June 2022].
- Levine, E., Mendonça, L., Baumal, C., Chin, A., Rifkin, L. and Waheed, N., 2020. Choroidal nonperfusion on optical coherence tomography angiography in a case of unilateral posterior segment ocular sarcoidosis misdiagnosed as MEWDS. American Journal of Ophthalmology Case Reports, 20, p.100944.
