Diya Baker (contact)
Birmingham Midlands Eye Centre
Syed Husain
College of Medical and Dental Sciences, University of Birmingham
Kim Lett
Birmingham Midlands Eye Centre
Rishika Chaudhary
Birmingham Midlands Eye Centre
Conflict of interest: No conflicts of interest are declared.
Funding: Nil
Introduction
Idiopathic macular holes (MHs) are most prevalent in the sixth and seventh decade of life with approximately two-thirds of patients being female, and can significantly impact patients’ quality of life. Although the aetiology is unknown, a range of risk factors have been proposed including; myopia, retinal detachment, hypertension and diabetic retinopathy (1). Classification of MH is important to determine treatment and prognosis (Table 1).
| Gass Stage | Description | Prognosis |
| 1 | 1a: Foveal detachment with lipofuscin coloured spot at fovea. 1b: Occult hole with lipofuscin coloured ring | 50% spontaneously close without treatment. 40% progress to full thickness MH. |
| 2 | Full thickness MH with diameter <400 microns, vitreous attached to macula | 15% spontaneously close without treatment. 75% progress. |
| 3 | Full thickness MH with diameter >400 microns, vitreous attached to macula. Operculum may be seen in front of lesion. | <5% spontaneously close without treatment. 50% progress. |
| 4 | Full thickness MH with diameter >400 microns, vitreous detached from macula. | <<5% spontaneously close without treatment. 20% progress. |
Table 1: Gass staging of macular holes (2)
Spontaneous closure, particularly in stage 3 and 4 idiopathic MH, is rare (3). Therefore, surgical intervention is indicated and routinely performed. Success rate following primary MH surgery is more than 90% (3-6). Nevertheless, the incidence of persistent MH post-operatively is reportedly between 4% and 13%. In cases of failed MH closure, re-operating is often considered standard practice (7,8).
We describe three cases in which spontaneous closure of MHs occurred following initial operation, thereby demonstrating scope for longer periods of monitoring prior to considering re-operation.
Case Descriptions
Case 1
An 84-year-old Caucasian male was referred for ophthalmic assessment following a routine optician appointment. The optician suspected a MH in the right eye. At the initial clinic visit, the patient presented with distorted vision for the past 6 months. There was no significant past ophthalmic or medical history.
On examination, Snellen best corrected visual acuity (BCVA) was 6/36 OD and 6/5 OS. Intraocular pressure (IOP) was 19mmHg in both eyes with Goldmann applanation tonometry. Anterior segment examination showed bilateral cataracts. Ocular Coherence Tomography (OCT) confirmed the diagnosis of a Gass stage 3, idiopathic full thickness MH (FTMH) in the right eye measuring approximately 517 microns.
Subsequently, he underwent uneventful routine right eye combined phacoemulsification with intraocular lens implantation, transconjunctival 23-gauge (23-g) pars plana vitrectomy (PPV) with internal limiting membrane (ILM) peel and gas tamponade. Posterior hyaloid face separation was achieved with aspiration and a core and peripheral vitrectomy was performed. Blue-dual was used to stain the macula. A high magnification BIOMâ lens was used to view the peeling procedure. The ILM was peeled by creating a flap with a MVR blade and then gently dissected with 23-g end-gripping forceps. A peel radius of approximately one-disc diameter was performed. Sixteen per cent C2F6 gas was used as the tamponade agent. Surgery was performed by an experienced surgeon under local anaesthetic. Post-operatively the patient was instructed to posture face down during the daytime and lie in a lateral position whilst sleeping for five days. He was prescribed guttae Maxitrol (dexamethasone, polymyxin B sulphate, neomycin) four times a day for 28 days and guttae Cyclopentolate 1% two times a day for 14 days.
Three weeks following surgery, BCVA was 6/60 OD and 6/4 OS. IOP in the right eye was 18mmHg. Dilated fundus examination showed a 30% gas fill and flat retina. The MH was 330 microns, open with elevated edges. A further six weeks later the MH had still not closed. The patient missed further follow-up appointments to discuss the option of re-operating and the emergence of COVID-19 further delayed these discussions. However, spontaneous closure of the MH unexpectedly occurred 10 months post-operatively.
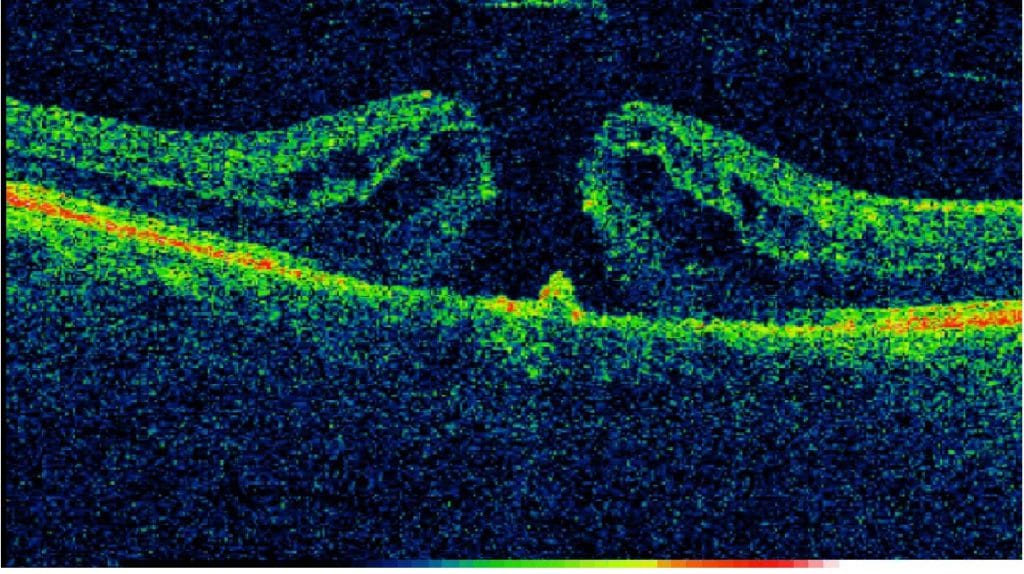
Figure 1: Pre-operative OCT scan
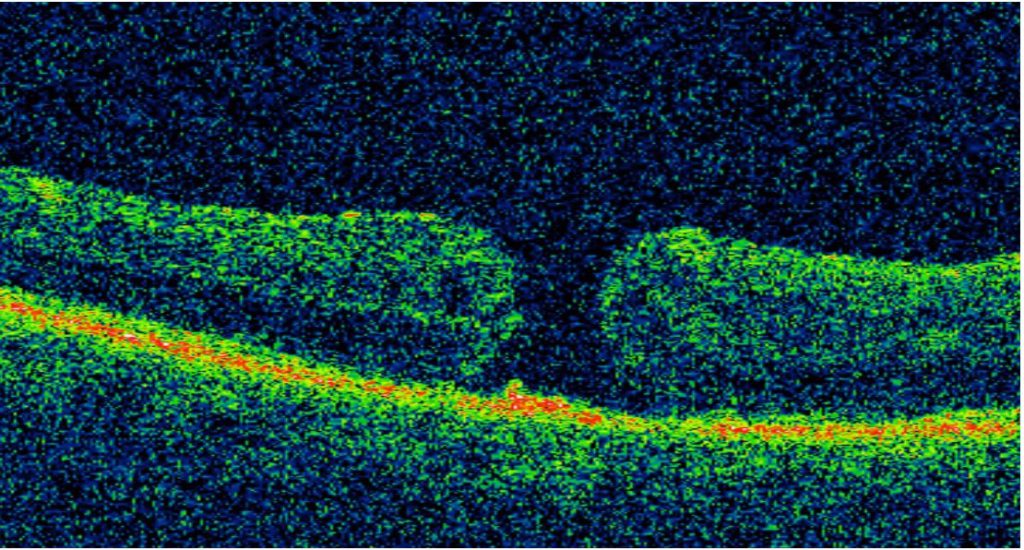
Figure 2: Immediate post-operative OCT scan
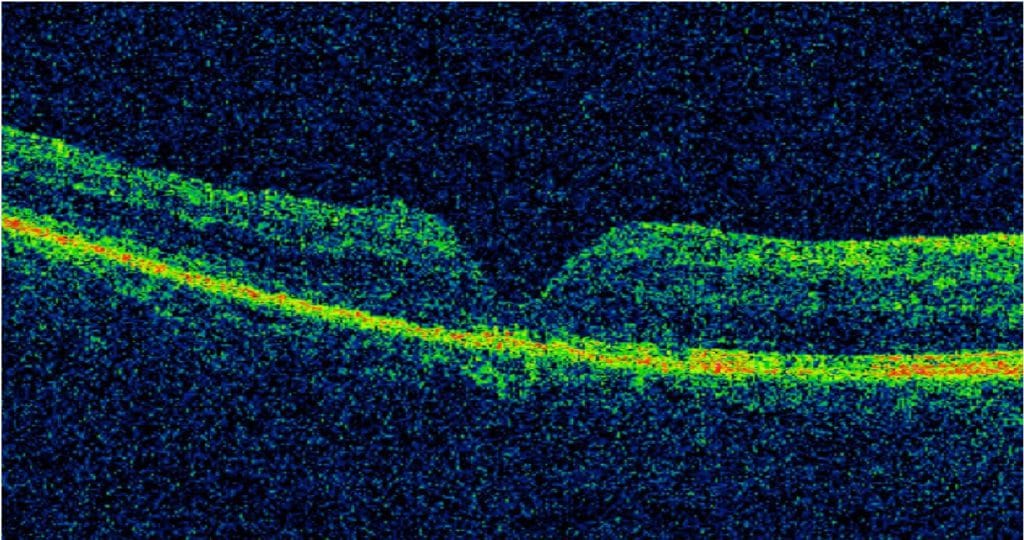
Figure 3: Following spontaneous MH closure
Case 2
A 72-year-old Caucasian female was referred from a routine optician appointment for further assessment of her retina due to visual deterioration in her left eye. The patient had no significant past medical history and a family history of glaucoma. Over a period of two months BCVA worsened from 6/6 to 6/18 OS. On slit-lamp examination the patient was found to have a left eye Gass stage 2 MH and a right eye partial thickness MH.
In the subsequent month the patient underwent left transconjunctival 23-g pars plana vitrectomy with ILM peel and C2F6 gas tamponade, however her vision remained unimproved at 6/18 OS due to the MH remaining open.
Approximately 11 weeks following surgery the patient noted that her vision had drastically improved in the last week. On examination the left eye MH was closed with BCVA 6/9. OCT of the left eye noted post-operative macula thickening and early epiretinal membrane.
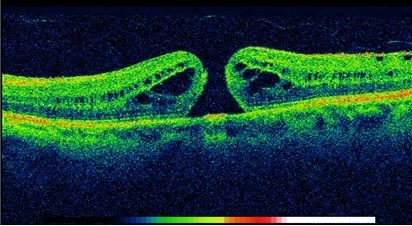
Figure 4: Pre-operative OCT scan
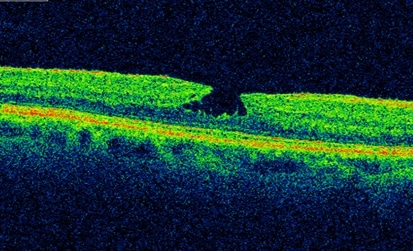
Figure 5: Immediate post-operative OCT scan
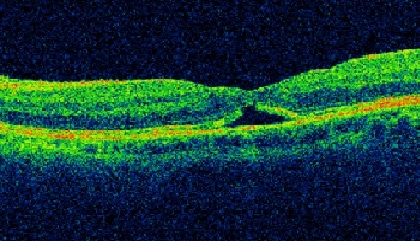
Figure 6: Following spontaneous MH closure
Case 3
A 54-year old Caucasian female was referred from a routine optician appointment following syncope and reduced visual acuity in the left eye. The patient had no significant past medical or ophthalmic history. A significant family history of glaucoma was noted. On examination BCVA was 6/24 OS. OCT imaging of the left eye showed a Gass stage 4 FTMH.
After 6 months, the patient underwent left 23-g PPV, ILM peel, C3F8 internal gas tamponade and retinopexy. During surgery, the retina was found to have multiple small tears and a small localised retinal detachment. The patient completed 7 days of face down posturing. Eight months following surgery the BCVA was 3/60 OS and the MH remained open.
The patient was keen for repeat surgery combined with phacoemulsification and intraocular lens insertion.
Approximately 8.5 months from initial surgery the patient attended for the pre-operative check and was found on OCT to have a spontaneously closed MH with a small outer lamellar defect.
Table 2: Table summarising cases in the series (OD- oculus dexter, OS – oculus sinister)
| Case | Gender | Age | Ethnic Back ground | Eye involved | Pre-op VA | Post- op VA | MH size pre-surgery (Microns) | MH size post-surgery (Microns) | Gas used | Delay until MH closure post operatively (weeks) | Time spent posturing (days) |
| 1 | Male | 84 | White -British | OD | 6/36 | 6/60 | 517 | 330 | C2F6 | 40 | 5 |
| 2 | Female | 72 | White- British | OS | 6/18 | 6/9 | 311 | Unable to measure to outer lamellar | C2F6 | 11 | 7 |
| 3 | Female | 54 | White- British | OS | 6/24 | 3/60 | 294 | Unable to measure due to hazy OCT view | C3F8 | 36 | 7 |
Discussion
Re-operation has shown limited visual and anatomical outcomes in patient with a background of previous failed MH surgery, despite this being considered standard practice. Currently the most recent literature does not offer clear consensus or recommendation regarding reoperation on persistent MHs (9). At best, Hillenkamp et al. elucidated in their retrospective study that macular hole configuration with the presence of a cuff of subretinal fluid at the break margins appears to be a strong prognostic indicator for anatomical closure and consequently advised retreatment in this patient sub-group (10).
Afrashi et al. reported an eight month delay in MH closure in a 57 year old female. In comparison to this case series, we found differences in patient’s age and demographics, absence of ILM peeling and larger pre-operative MH size (671 microns); the latter two being recognised as poor prognostic factors (11,12). In this case series, all patients had gas tamponade (C2F6 or C3F8), which is likely to increase closure rates, particularly for MHs greater than 400 microns. Furthermore face-down posturing was applied in all our cases, despite benefits only clear for MH larger than 400 microns (12-14).
Our case series highlights an essential question regarding the physiological processes involved in delayed spontaneous MH closure. Undertaking a literature search revealed multiple hypotheses for mechanisms which may cause spontaneous late closure of MHs following surgical intervention.
ILM peeling may potentially facilitate early closure by promoting natural glial cell proliferation. However, there is minimal evidence to explain the reasons for the extended post-operative recovery, or the specific triggers which promote glial cell proliferation (15).
An observational study performed by Michalewska et al. showed a correlation between the shape of MH edges and spontaneous MH closure (3). On OCT scans, MHs with irregular edges were found to have a higher chance of spontaneous MH closure as compared to smooth edged MHs. We postulate that these irregularities induce migration of Müller cells (retinal glial cells) and initiate a bridging effect eventually resulting in closure of the MH (16).
The longest reported duration before spontaneous closure of FTMH is approximately 28 months (16). We have shown large variation in closure of MH between 3 months and 11 months. Since all patients in our case series had intact outer retinal layers, this suggests the extent of improvement in VA may be related to the preservation and/or restoration of the outer retinal layers in FTMH.
We also propose that surgery on the retina may induce cell growth; operations on MHs stimulate a concentric pattern of growth around the edges which bridge neuroretinal tissue over the MH. This concentric growth may progress over a period of time in a chain reaction (domino effect) of glial cell proliferation. Yet, the reason as to what specifically generates this process and why this takes long periods of time are questions which remain unanswered.
How long should clinicians wait before reoperation? Schuman et al. suggest a waiting period of 6 weeks prior to re-operating in idiopathic MHs (7). This time-period likely requires revision since all our cases closed significantly later than the suggested 6 weeks.
Conclusion
In order to prevent unnecessary additional operations, delayed MH closure is important to consider prior to reoperating. Perhaps instead of focusing on reoperation, scheduled rigorous follow up investigations with OCT is more appropriate. Time-lapsed sequential SD-OCT imaging may further elucidate and confirm the basic physiological processes for spontaneous MH closure and delayed MH closure (9).
Learning points
- Importance of recognising potential late closure of MHs and allowing sufficient time for closure to occur before re-operating.
- Counselling patients prior to MH closure surgery about the potential risk of delayed MH closure and the need to weigh this possibility against re-operating in the case of a persistent MH.
- Use of time-lapsed sequential OCT images in patients with MHs, may offer a greater understanding of delayed MH closure.
References
- Cour ML, Friis J. MHs: classification, epidemiology, natural history and treatment. Acta Ophthalmologica Scandinavica. 2002;80(6):579–87.)
- Gass JD. Idiopathic senile MH. Its early stages and pathogenesis. Arch Ophthalmol 1988;106:629-39.
- Michalewska Z, Cisiecki S, Sikorski B, Michalewski J, Kałuzny JJ, Wojtkowski M, et al. Spontaneous closure of stage III and IV idiopathic full-thickness MHs–a two-case report. Graefes Arch Clin Exp Ophthalmol. 2008 Jan;246(1):99–104.
- García-Pous M, Udaondo-Mirete P, Amselem-Gómez L, Salom-Alonso D, Cervera-Taulet E, García-Delpech S, et al. [Spontaneous resolution of idiopathic MH type IV: optical coherence tomography follow-up]. Arch Soc Esp Oftalmol. 2006 Apr;81(4):229–32.)
- Smiddy WE, Feuer W, Cordahi G. Internal limiting membrane peeling in MH surgery. Ophthalmology 2001;108:1471–6.
- Min WK, Lee JH, Ham DI. MH surgery in conjunction with endolaser photocoagulation. Am J Ophthalmol 1999;127:306–11.
- Schumann RG, Rohleder M, Schaumberger MM, Haritoglou C, Kampik A, Gandorfer A. Idiopathic MHs: ultrastructural aspects of surgical failure. Retina. 2008;28:340–349.
- Reid GA, McDonagh N, Wright DM, Yek JTO, Essex RW, Lois N. First failed MH surgery or reopening of a previously closed hole. Do We Gain by Reoperating?—A Systematic Review and Meta-analysis. RETINA. 2020 Jan;40(1):1–15.
- Falkner-Radler CI, Gabriel M, Binder S. Spontaneous closure of an idiopathic MH 9 months after unsuccessful vitreoretinal surgery. Retin Cases Brief Rep. 2014;8:157–60.
- Hillenkamp, J., Kraus, J., Framme, C., Jackson, T., Roider, J., Gabel, V. and Sachs, H., 2007. Retreatment of full-thickness macular hole: predictive value of optical coherence tomography. British Journal of Ophthalmology, 91(11), pp.1445-1449.
- Afrashi F, Öztaş Z, Nalçacı S. Late Closure of a Stage III Idiopathic MH after Pars Plana Vitrectomy. Turk J Ophthalmol. 2015 Dec;45(6):274–6.
- Mester U, Becker M. Prognostic factors in surgery of MHs. Ophthalmologe 1998;95:158–62
- Madi HA, Masri I, Steel DH. Optimal management of idiopathic MHs. Clin Ophthalmol. 2016 Jan 13;10:97–116.
- Gaudric A: Macula hole surgery: simple or complex? Am J Ophthalmol 2009;147:381–383.
- Schweitzer, K. D., & García, R. (2007). Spontaneous closure of a stage III idiopathic MH. Canadian Journal of Ophthalmology / Journal Canadien d’Ophtalmologie, 42(1), 127–128. doi:10.3129/can.j.ophthalmol.06-107
- Patel, R., Gopalakrishnan, M., Rajesh, B. and Giridhar, A., 2017. Postvitrectomy macular hole undergoing delayed closure after 28 months. Indian Journal of Ophthalmology, 65(9), p.882.
